The new coronavirus that has infected millions of people around the globe can wreak havoc far beyond the lungs. Some of the symptoms of the disease it causes, COVID-19, are predictable enough: cough, fever, chills, headache. But the pathogen’s effects by no means stop there. The virus can cause problems in almost every organ, including the brain, heart, kidneys, gastrointestinal tract and skin.
Physicians have been taken aback at what they now call silent hypoxia, or happy hypoxia, a phenomenon in which people with dangerously low levels of blood oxygen are astonishingly not struggling to breathe. And there is “COVID toe,” painful swellings on the skin called chilblains. In rare cases, children—who were previously thought to be relatively spared from severe illness—come down with symptoms akin to Kawasaki disease, which leads to inflamed blood vessels throughout the body. Complications associated with blood clots, such as strokes and pulmonary embolisms (blockages of blood vessels in the lungs) also turn up. “It’s interesting that a respiratory virus will cause such a diverse array of clinical sequelae,” says Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine.
One of the reasons for the unusual manifestations of COVID-19 may simply be the more than four million confirmed cases worldwide of a wholly new illness. Some of these symptoms have appeared during other viral infections—for example, researchers have seen blood clots in some patients infected with the original SARS coronavirus and the H1N1 influenza virus. “There are so many cases in the world now that we may be picking up on minor variants,” says Stanley Perlman, a professor of microbiology and immunology at the University of Iowa. “It makes you wonder, if in other infections, you look at two [million] to three million [cases], how many of these kinds of events would occur. Or is [the situation] really special for COVID-19?”
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
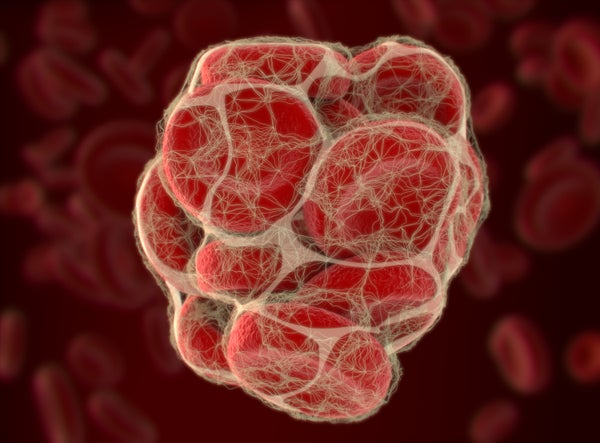
Scientists are still trying to pin down the exact mechanism underlying the wide range of complications. There seem to be two key leading suspects, however. The first is the immune system’s defensive inflammatory response to foreign invaders such as viruses and bacteria. That reaction, in turn, may lead to the second culprit: blood clotting. The disease’s impact on blood vasculature appears to underlie some of the more bewildering effects COVID-19 patients encounter.
Reports of clotting-related complications such as pulmonary embolism and stroke among COVID-19 patients in intensive care units have come from several countries, including China, France, Italy and the U.S. The overall frequency of such issues remains unclear, but some assessments suggest that they appear in as many as 30 percent of critically ill patients. In rare cases, strokes have turned up in people in their 30s and 40s, alarming doctors.
“We’re seeing lots of different coagulation abnormalities” in the patients admitted to the ICU, says Margaret Pisani, an associate professor specializing in pulmonary and critical care medicine at the Yale School of Medicine. “We’ve seen strokes, myocardial infarctions, pulmonary embolisms—clots in places that we don’t normally see in otherwise healthy people who come in with a viral infection.”
Clotting-related issues are not specific to COVID-19, says Yvonne Maldonado, a professor of pediatric infectious diseases at Stanford University. A condition known as disseminated intravascular coagulation, in which abnormal clotting occurs throughout the blood vessels, has previously been reported in patients with infectious diseases who experience sepsis (a life-threatening immune response to a contagion). “What’s unusual here is that it is seems to happen with this disease more often than with other diseases,” she says.
In addition to clots in large blood vessels, researchers have reported clotting within smaller blood vessels known as capillaries. COVID-19 “is a vascular problem” says Frank Ruschitzka, a cardiologist at University Hospital Zurich. “The lung is the main battlefield, but it’s a disease of the blood vessels.”
Scientists have yet to pin down the cause of the clotting. Inflammation appears to be a likely culprit, however. Researchers have found, for example, the presence of complement proteins—molecules involved in activating the immune response—within clotted blood vessels. Across many of COVID-19’s myriad symptoms, the common mechanism appears to be the inflammation of the endothelium, the layer of cells that make up the inner lining of blood vessels, says Luciano Gattinoni, a visiting professor in the departments of anesthesiology and intensive care at the University Medical Center Göttingen in Germany. “As the endothelium is present everywhere, you can explain why the symptoms are so different.”
Some of the mysterious symptoms linked to COVID-19 start to make sense when they are viewed as manifestations of a vascular disorder. Take silent hypoxia, a condition Gattinoni has drawn attention to in recent weeks as being unrelated to lung oxygen capacity but rather to impaired blood flow through the organ.
Many other odd manifestations of COVID-19, including thekidney problems that require dialysis (in some cases, clotted blood has reportedly
clogged filters in dialysis machines),chilblains in toes and Kawasaki-like symptoms in children, have been associated with vascular complications as well. “This is an extremely rapidly evolving field, but the vascular component of the disease is obvious,” Ruschitzka says —although he cautions that “there is never one mechanism alone.”
Whether the vascular problems associated with COVID-19 arise from direct effects of the virus or the body’s immune response remains an open question. Some evidence suggests that SARS-CoV-2, the coronavirus behind COVID-19, can directly attack the endothelial cells. In April Ruschitzka and his colleagues published a paper that chronicled three autopsies in the Lancet that found the presence of viral particles in the endothelia of kidneys and an accumulation of inflammatory immune cells within the endothelia of various organs, including the kidney, heart and lungs. Ruschitzka, however, says that that the body’s immune response, not the virus itself, is the more likely explanation for the excessive clotting. “What we see everywhere is pronounced inflammation,” he adds.
Still, it is too early to rule out direct effects of the virus. “There are a lot of conditions that cause inflammation where you don’t see these kinds of clotting disorders,” Hotez says, raising the prospect that the virus may be directly involved in spurring blood abnormalities. The diversity of symptoms, he suggests, may have to do with the ACE2 receptors that SARS-CoV-2 binds to. These receptors are present on the surfaces of cells of multiple organs affected by COVID-19.
Alex Richter, an immunologist at the University of Birmingham in England, notes that the timing of a symptom may hint at whether it is caused by the virus itself or the body’s immune response to it. A frequent early symptom—the loss of taste and smell—may more likely be a direct effect of the virus than the clotting complications or Kawasaki-like symptoms that appear later. “There’s almost a time line of how we’re getting these symptoms and how likely they are to be a direct effect of the virus or because of a hyperimmune response,” she says.
Richter notes that what is particularly strange about the Kawasaki-like symptoms seen in children is that they seem to appear several weeks after initial exposure to the virus. She and her team are currently investigating samples from affected children to pinpoint how the immune system might be generating these effects. So far, they have found evidence that these individuals possess antibodies suggestive of a well-developed immune response, indicating that the infection likely occurred weeks prior to the onset of symptoms. Richter says this observation is distinct from what has been seen in adult cases, in which the immune system seems to be reacting much more immediately to the contagion.
Despite the wide range of COVID-19 symptoms, the emerging understanding of the infection hints at a set of common underlying factors that may be at work. “It could be that it’s actually just a few things that are going on, and depending on where they manifest, you see all these different symptoms,” Perlman says. “Then the question is: why does it manifest differently in different people?” Most people who are infected with SARS-CoV-2 will not need to be admitted to the ICU, but those who are hospitalized confront an illness that continues to hold surprises for the medical community. Clear risk factors presage severe disease, including age, obesity and heart conditions.Butscientists are still looking for inflammatory biomarkers and other biochemical signposts to help physicians predict who will get better on their own and who will become severely ill, Maldonado says, adding: “Everybody’s trying to figure that out.”
Read more about the coronavirus outbreak from Scientific American here. And read coverage from our international network of magazines here.