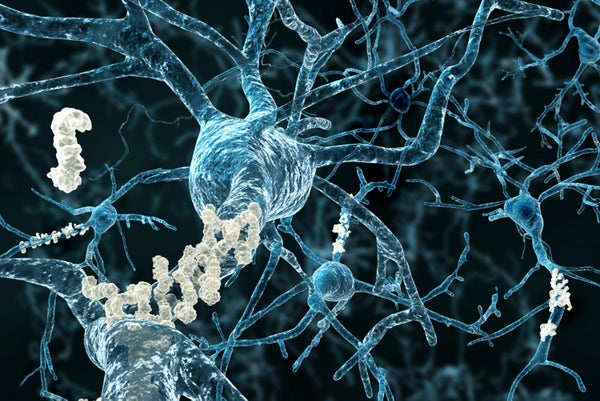
To many of us, Alzheimer’s disease is a familiar and terrifying malady. Afflicting an estimated 5.3 million people in the U.S. alone, the disorder slowly and relentlessly robs patients of memory, judgment and perception—eventually corroding even their ability to perform everyday tasks. The mechanisms that underlie these symptoms are not yet fully understood. The disease is largely attributed to an abnormal buildup of proteins, which can form amyloid beta plaques and tangles in the brain that trigger inflammation and result in the loss of brain connections called synapses, the effect most strongly associated with cognitive decline.
In a study published this week in Science, a team of researchers led by neurologist Beth Stevens at Boston Children’s Hospital has found evidence that such synapse loss may in fact occur much earlier in Alzheimer’s disease. Rather than being a secondary effect of these protein pathologies, as experts had previously thought, this process may begin well before plaques form.
Synapse elimination, or “synaptic pruning,” is a normal process that occurs during development—and one that Stevens has been fascinated by for years. She has found some proteins that initiate an immune response to clear the body of any harbinger of illness also play a role in tagging weak or unwanted synapses for elimination. This process allows specialized Pac-Man–like brain cells called microglia to engulf the targeted synapses, paving the way for more precise brain wiring.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Throughout our lives the brain’s junctions are trimmed and pruned—a process that is crucial to normal development. Stevens and her team suspected that the mechanisms involved in such pruning might be aberrantly turned back on—hijacked, so to speak—to contribute to synapse loss in Alzheimer’s. “That’s what makes us unique in the way we’re approaching this problem,” she says. “A lot of work that initiated this project stemmed from what we learned about how these pathways work in normal brain development, and as we learn more about how it normally works we think it’ll provide us with novel insight about how to target it in disease.”
The researchers tested their theory using mouse models of Alzheimer’s, employing high-resolution imaging techniques to pinpoint when and where synapse loss occurred. In this rodent model there was a window of time before plaques would appear, during which the researchers observed that the mice were losing synapses in the hippocampus, a brain region responsible for memory and learning.
What was particularly striking, Stevens notes, is that the researchers also found high expressions of C1q, a protein involved in normal synaptic pruning. “So we wanted to know: Could [such proteins] be contributing to synapse loss in these models?” she says. The researchers knocked out the genes for C1q and C3 (a protein activated by C1q) and found that by doing so, they had protected the mice’s synapses.
To better explain this finding, the team turned to yet another protein, amyloid beta—which in its soluble form, before building up and hardening into plaques, has already been found to be toxic to the synapses. The researchers delivered this toxic form of amyloid beta to three groups of mice: a normal control group, a group that genetically lacked C1q and one treated with an antibody that blocked the function of C1q in the brain. In the first group extensive synapse loss occurred in the hippocampus—loss that did not occur in the mice in which C1q had been inhibited. “This showed us that C1q and amyloid beta were working together in the same pathway,” Stevens says. “That C1q is necessary for amyloid beta to cause this damage.” Using this experimental model, the researchers then observed the behavior of the microglia and found that the soluble form of amyloid beta stimulated microglia to engulf synapses. Inhibiting C1q, however, protected against this effect.
“This study is a major advance in our understanding of the molecular mechanisms underlying Alzheimer’s, in demonstrating a causal role for immune molecules in this disease,” says Kimberley McAllister, a neurobiologist at the University of California, Davis, who did not participate in the research. “It’s really exciting to me,” adds Tara Spires-Jones, a neuroscientist at the University of Edinburgh, also unaffiliated with the study. “It’s bringing together two parts of the field…synapse loss and inflammation problems are linked.”
Manuel Graeber, a neuropathologist at the University of Sydney who did not take part in the study but has worked extensively with microglia, believes these findings will also play an important role in focusing scientists’ attention on these cells’ function. “The paper highlights this maintenance system of the brain that’s not sufficiently appreciated,” he says. Generally researchers associate these cells with an immune response; however, the work by Stevens and her colleagues reveals these same cells in a different light. “And I think it will help correct [that] misconception.”
Stevens’s team believes their results have implications that extend far beyond Alzheimer’s disease. Because synapse loss plays a role in a wide range of other disorders such as autism, schizophrenia, Huntington’s and glaucoma, “we’re excited about the possibility that this is a more global mechanism, that it’s not disease-specific,” Stevens says. She has already begun testing this idea in other disease models.
A recent study linking schizophrenia and variations of the gene C4 also implicates the pathway involved in synaptic pruning. “These findings suggest that new therapeutics targeting this pathway could treat a broad range of neurodegenerative and psychiatric disorders,” McAllister says.
Developing such treatments, however, remains far in the future. The researchers first need to test their findings in humans—and there are other factors to consider. For example, they have not yet determined the mechanism responsible for initially switching C1q on. That factor, Stevens says, “may be relevant to a lot of diseases—something upstream we can also think about targeting,” Stevens says. C1q also plays a positive role in the brain by clearing out dead cells and helping target harmful materials, so learning how to manipulate its presence to prevent debilitating synapse loss while maintaining its normal functions will require further research.
Furthermore, other research groups have identified different avenues for targeted therapy. In another rodent study published this week in Science Translational Medicine a group of researchers from multiple institutions identified a pathway responsible for the formation of amyloid plaques. More specifically, they found that heparan sulfate, a class of molecule found on the surface of cells (including neurons), essentially “traps” amyloid peptides, causing them to aggregate and form deposits that will eventually lead to neurodegeneration and dementia. When the research team deleted a gene that allows heparan sulfate to adhere to the surface of neurons, they found much less amyloid plaque. “Rather than using an immune method or targeting an enzyme, which have side effects, we want to target this specific pathway so that the brain can naturally clear amyloid-beta peptides when they’re not trapped by heparan sulfate,” says Guojun Bu, a neuroscientist at Mayo Clinic in Jacksonville, Fla., and the study’s lead author.
Similarly, Stevens is optimistic about the future utility of her findings for developing therapies. “C1q seems like a good target,” Stevens says. “We don’t have evidence that [such proteins are] driving the whole process but we think it’s an early part, and if you knock it out or manipulate it, you could have the promise of an early impact and protecting at least the synaptic part of the story.”