The Ebola outbreak in the Democratic Republic of the Congo (DRC) just got worse. In what the World Health Organization’s top response official is calling a “game changer” event, one case has now been confirmed in Mbandaka—a city of 1.2 million people about 150 kilometers from the rural rainforest area where the other confirmed Ebola cases have been found.
The country has been grappling with 44 reported cases, three of which have been confirmed. Another 20 of these cases have been categorized as probable, and 21 are suspected. At least 23 of these individuals have died, according to the latest WHO figures.
The Geneva-based Gavi, The Vaccine Alliance, a public-private partnership that has purchased 300,000 doses of the experimental Ebola vaccine for an emergency stockpile, has already committed funding to deploy thousands of doses during this outbreak. This Merck-produced vaccine has been through clinical trials but is not yet licensed by any health authority. The DRC government, however, approved its deployment under what are known as compassionate-use regulations.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
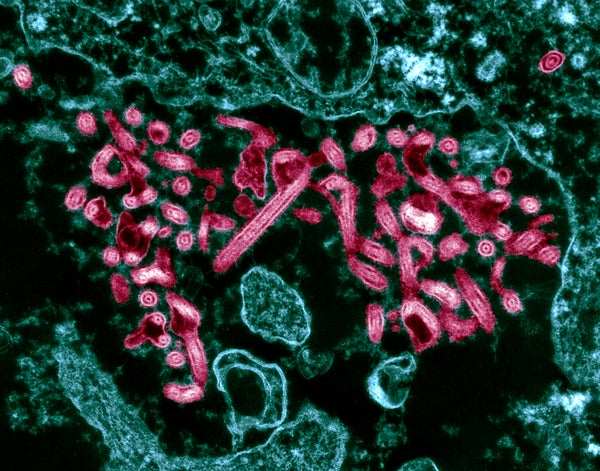
Public health workers are now racing to quarantine potential cases in an attempt to limit the disease’s spread. They are also trying to identify all the people who may have been in direct contact with someone who is infected, so they can start inoculating them with the experimental Merck vaccine as early as this weekend. That shot consists of Ebola surface proteins spliced to a live virus that causes the livestock disease vesicular stomatitis.
Seth Berkley, an infectious disease epidemiologist and the chief executive of Gavi, spoke with Scientific American about the latest developments in the outbreak, and about the vaccine response plans.
[An edited transcript of the interview follows:]
What’s the current situation on the ground in the DRC, now that there is at least one case in an urban location?
You have to remember urban depends on how you define urban—this is not Washington, D.C. This case is definitely more worrying than one in a very remote, isolated location, however. The issue now is that we have seen Ebola in multiple areas, and that certainly increases the risk of transmission and therefore increases our worries. The hope is that by early intervention and engagement, this outbreak can be controlled. Of course, if necessary, the company [Merck] could start making more vaccine.
How many doses of vaccine have arrived so far to the DRC, and how many more can GAVI support?
On the ground now are 4,320 doses and another 5,400 doses are moving towards there. That means within a few days we should have more than 9,000 in the DRC. When we did our advance purchase commitment with Merck they were required to have 300,000 doses available, so there are obviously more doses that we can move forward if necessary.
This experimental vaccine can only be used in the context of a clinical trial. Can you talk a bit about that?
This vaccine—and only this vaccine—has been through efficacy trials in humans and there it showed 100 percent efficacy protecting against Ebola. But the point is that it has gone through all of those procedures and is now being prepared for licensure. In a sense it is an experimental vaccine because it is not yet licensed—but you also need to keep in mind that it is a vaccine that has gone through safety and efficacy testing already. This clinical trial will provide more data on safety and efficacy, and will be done under informed consent using good clinical practices.
What is the makeup of the clinical trial?
This is not a trial to ask the question, “Does the vaccine work or not work?” because we already have information on that. The finalization of the protocol is going on now, as we speak, so I don’t want to go into details until it is finalized. But basically it is going to be a “ring vaccination” approach, which means that once there are known Ebola cases then all of those individuals’ contacts, family members and so on will be vaccinated and will then will be followed up on, on a regular basis. The vaccination efforts will also include health workers. Exactly how far those efforts will extend out will be decided on the ground—like if it will include burial workers, first responders, etcetera.
The vaccine was found to be 100 percent effective in field tests in Guinea in 2016, meaning none of the vaccinated people came down with the disease whereas unvaccinated people did. Is there any reason to think the situation might be different here?
It is the same strain of Ebola—Ebola–Zaire. Of course, it is always possible that there are different factors that can affect people’s uptake of vaccine, so in a sense you always have to watch out for that in a new population. This vaccine was used in a field setting in west Africa, however, so it’s not like this was a vaccine tried in a completely different place and situation.
What are the challenges deploying this vaccine on the ground?
The biggest challenge is the logistical challenge. The original area this was found in the DRC is not easily reachable and now it has been found in a number of places. My understanding is thatat least one of the cases was related to a funeral, though I haven’t confirmed that myself. So tracking this is difficult, and it is about shoe leather epidemiology—asking who might have been in contact with cases in a very stressful time.
The vaccine itself must be stored at –70 degrees Celsius or –80 degrees C, so that is an issue in terms of transport. Luckily there are good transport and portable transfer tools to do that. It can be used for a couple of weeks at normal, refrigerated settings on the field—but that’s a challenge, too, [because electricity can be unreliable]. Getting teams together who will ensure there is informed consent is a challenge as well.
The vaccine only works against one of the most common strains of the Ebola virus—the one apparently circulating in the DRC. Is there concern about this strain mutating in a way that would render the vaccine unhelpful, and are there any genome-sequencing efforts ongoing in real time to track the viral changes?
Right now people are trying to figure out what is going on there. I don’t think any real-time genome sequencing is going on right now, and you have to understand this is one of the most isolated places on Earth—which means things have to be delivered by helicopter and boat.
Are you preemptively sending vaccine doses to neighboring countries?
No, at this point it’s not being sent to other locations. Obviously the WHO and the DRC government are putting out warnings for travelers and trying to set up controls over crossing borders. But this is hard to do in such an isolated rainforest area.
Do you expect anyone to refuse the vaccine?
It hasn’t been offered to anyone yet. It will hopefully be offered at the end of this week or the beginning of next week. At that time, we will look closely at the acceptance rate. My guess is that since this disease and its effects are known that it will be welcome. One issue will be how do you make sure it is available to the people it is indicated for [meaning direct contacts of the ill and health workers]—and not the worried well.
Another question going forward will be how do we protect health workers. We may want to keep health workers prophylactically vaccinated, but that’s not on the table yet. Right now it’s a matter of responding to the emergency.