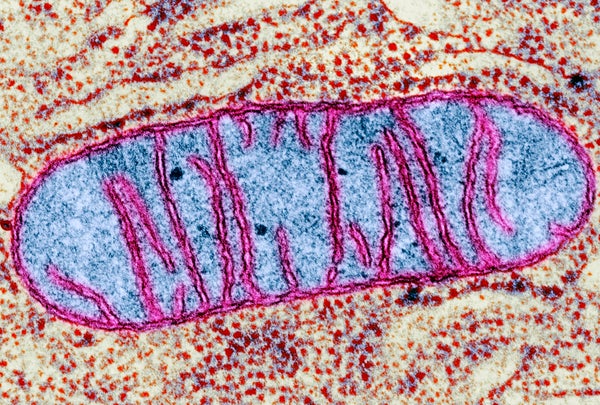
Researchers have long believed that problems with mitochondria—the power plants of cells—underlie some cases of Parkinson’s disease. Now a new study details those problems, and suggests that they may form a common thread linking previously unexplained cases of the disease with those caused by different genetic anomalies or toxins.
Finding a common mechanism behind different suspected causes of Parkinson’s suggests that there might also be a common means to measure, treat or cure it, says Marco Baptista, research director at the nonprofit Michael J. Fox Foundation, a leading center for study and advocacy in the fight against Parkinson’s.
The study, published Thursday in Cell Stem Cell, did identify a possible way to reverse the damage of Parkinson’s—but only in individual cells and fruit flies. Finding a treatment that does the same thing in people will be challenging, Baptista says.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Roughly one million Americans have Parkinson’s disease, which is characterized by motor problems and can cause other symptoms including cognitive and gastrointestinal difficulties. About 1 to 2 percent of cases are linked to mutations in the LRRK2 gene, with far fewer associated with genes known as PINK1 and Parkin. Exposure to environmental factors such as toxic chemicals can also lead to Parkinson’s, although most cases have no obvious cause.
In the new paper Xinnan Wang, an assistant professor of neurosurgery at Stanford University, and her colleagues show that mitochondria are underpowered in several types of Parkinson’s and that these mitochondria also release toxic chemicals. Looking at fly models of the disease as well as cells taken from patients, the researchers found that they could correct these problems and reverse neurodegeneration if they reduced levels of a protein involved in mitochondrial activity. “I think it’s a really cool piece of work,” says Thomas Schwarz, a professor of neurology and neurobiology at Harvard University who was not involved in the research but was Wang’s postdoctoral adviser.
It had been clear that Parkinson’s cases caused by toxins, or by Parkin or PINK1 mutations, involved mitochondria problems, Schwarz says. But the new paper shows that Parkinson’s driven by the LRRK2 gene is also subject to the same mechanism and hints that unexplained cases may also involve the same difficulties in clearing faulty mitochondria from cells. “Here’s the best evidence yet that even those forms are some sort of mitochondriopathy,” Schwarz says. “Seeing those completely disparate, unrelated spontaneous cases—linked up to this question of how are mitochondria cleared and how is their movement controlled—is absolutely fascinating.”
One question that remains is why would a general problem of cellular physiology cause Parkinson’s? Both Schwarz and Wang have hypotheses: Wang says that the brain cells whose degeneration leads to Parkinson’s—the cells that control release of the neurotransmitter dopamine—are particularly energy-dependent and vulnerable to stress. Deprive a skin cell of energy and it won’t work as efficiently; deprive a dopaminergic neuron of energy and it may die, she adds.
Schwarz says these neurons are also distinctive in their anatomy. They have so many branches linking them to other brain cells that they can extend up to 4.5 meters in length. Mitochondria are distributed along these branches and must continually be refreshed, with old ones cleared out on the order of some 33,000 mitochondria per cell each day. “That’s just a staggering burden for the cell to carry,” says Schwarz, who in his own research explores how mitochondria move along these axons. “That’s why even a minor slowing or defect in the way the mitochondria are cleared out, or damaged proteins are dealt with, winds up being a major crisis for a cell that has 4.5 meters of axon, compared to a liver cell or even your average neuron elsewhere in the brain.” Figuring out a way to measure this overload before it brings about symptoms of Parkinson’s might lead to earlier diagnoses, before irrevocable damage is done, he adds.
The paper released Thursday addresses the mystery of how Parkinson’s caused by PINK1 and Parkin mutations, which are known to affect mitochondria, could share the same symptoms as those caused by mutations in the LRRK2 gene, which is involved in how cells take out their trash. Wang and her team found that problems turn up when spent mitochondria are not cleared properly from the cell, a situation that provides a link between the two problems. The different mutations may act on the mitochondria differently but both end up causing the same mitochondrial dysfunction, Wang says. These dysfunctional mitochondria also produce toxins, much like a power plant does, she says, further damaging the cells.
Asa Abeliovich, a pathologist and neurologist at Columbia University who was not part of this study, says the paper effectively links these two genetic routes to Parkinson’s: the garbage disposal problem and the toxic accumulation that occurs when cellular energy plants go awry. Abeliovich, however, thinks it is still speculative to conclude these problems are also to blame for the noninherited cases of Parkinson’s.
Wang agrees that she needs to test her theories in other models of Parkinson’s before declaring that a cure might lie in fixing mitochondrial problems. Just because the team found the mitochondrial problems in human cells and in a fly model of Parkinson’s “doesn’t necessarily mean that in humans it is the cause [of Parkinson’s],” Wang says, “but suggests it is a possibility—[and] suggests a future direction to look in human patients and see if lowering this protein has any therapeutic benefits.”