Over the last few decades, researchers tinkering with molecules that turn an immune cell on and off have created a revolutionary approach to fighting cancer. Instead of taking aim at the tumor directly, this new class of medicines harnesses the patient’s own immune cells to tackle the disease. Immune-based cancer therapies are saving thousands of lives, and the science behind them earned the 2018 Nobel Prize in Physiology or Medicine.
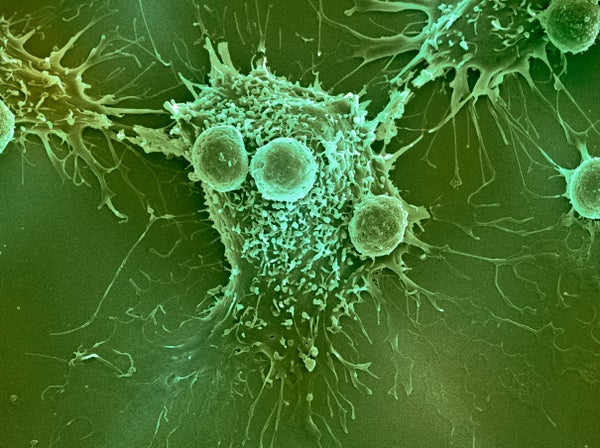
These drugs, called checkpoint blockers, appeared after scientists discovered molecules that help cancer cells block immune processes that would otherwise attack a tumor. The secret lies with several “brake” proteins on white blood cells, T cells, that prevent the immune system from overreacting to microbial threats. Tumor cells have learned to survive by engaging the brake molecules, sending T cells into a stupor that allows cancer to gain a foothold. By thwarting this hijacking maneuver, checkpoint blockers release the brakes and awaken T cells to attack the tumor. A clever trick—except that so far, these immune-based drugs only work in about a fifth of cancer patients and for certain tumors, barely at all.
To push past those limits, a few companies are venturing into a new frontier—glycobiology, the science of the sugars that stud the surface of cells. Sugars act like switches and knobs that control where and when a cell’s biological machines, proteins and lipids, do their jobs. Yet for all their fine-tuning finesse and power, sugars are highly complex molecules that have often eluded a deeper understanding of their workings because they are so hard to study in the lab.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Recently, though, the science has caught up and biotech companies have begun to build on these findings to develop anti-cancer drugs. In November at an American Association for Cancer Research meeting in Miami, Palleon Pharmaceuticals, a Massachusetts startup, unveiled new data from experiments in rodents on a profoundly different set of checkpoint blockers that target sugars.
These experimental drugs work by interfering with complex sugars called glycans that coat the surface of tumor cells and let them pass unnoticed by the otherwise vigilant immune system. It’s an “underappreciated mechanism of immune evasion,” says Michael O’Dwyer, a clinician-researcher at National University of Ireland, Galway, who has no ties to Palleon. Many researchers are going after the T cells’ braking systems, he says, but “probably with diminishing returns.” He adds: “There’s only so much you can get out of the T cells.”
Jim Broderick, chief executive and founder of Palleon, compares the immune system to a football team. Defending against threats—whether bacteria, viruses or cancer—requires a coordinated effort from many cell types with different roles. Following the game analogy, the current wave of cancer immunotherapies focuses on the quarterback. “But Tom Brady can’t win the Super Bowl if he has third graders on his offensive line,” Broderick says.
Palleon launched in 2015 on the strength of research by a handful of labs suggesting that structured patterns of cell-surface glycans—a molecular fingerprint on virtually all cells—might hold the key to rousing a host of additional cancer-fighting immune cells. These macrophages, natural killer cells and other cells make up a different arm of the immune system. Known as innate immune cells, these cells form the body’s first line of defense, which sets the stage for a subsequent T-cell attack.
One particular glycan, sialic acid, is sensed by a family of surface proteins found mostly on innate immune cells but also on activated T cells at tumor sites. These proteins, called Siglecs, act as molecular brakes. When Siglecs bind to sialic acids, coating the surface of a tumor, the immune cell goes to sleep. Several companies—including Innate Pharma in Marseille, France, and South San Francisco–based Alector—are hoping to wake those drowsy cells with therapies that block Siglecs.
A team of researchers led by Palleon co-founder Carolyn Bertozzi, a Stanford chemist, went after these same molecular pathways with a radically different approach. Rather than trying to block individual Siglec molecules on the surface of immune cells, the researchers designed a therapeutic that stymies all Siglecs by trimming sialic acids off the tumor cell. In a 2016 proof-of-concept study, the team showed that treating a dish of breast cancer cells with the experimental drug exposed them to killing by natural killer cells.
At another immunotherapy meeting in Washington, D.C. in November, Palleon vice president Li Peng presented data showing this strategy can work in mice with implanted tumors—even in ones that draw weak responses with FDA-approved checkpoint-blocking drugs. In separate experiments, the team confirmed that T cells, macrophages and natural killer cells all contribute to the drug’s benefit. Cancer cells “are like wolves in sheep’s clothing—bad guys disguising themselves with the glycan code,” Peng says. By removing sialic acids from glycans on the surface of tumor cells, the drug “reveals their real identity so immune cells can see the bad guys.”
Dong Zhang, director of immunology at the German company EMD Serono, considered Peng's talk “one of the most exciting findings” at that meeting.
To make the original version of the therapeutic, Bertozzi and colleagues chemically fused the sialic acid–trimming enzyme to an antibody that recognizes a hallmark protein (HER2) on the surface of breast cancer cells. The antibody is needed to restrict the enzyme’s activity to the tumor. Otherwise the enzyme would cut indiscriminately and wreak havoc, since sialic acids also play vital roles on healthy cells.
With an eye toward human trials by 2020, Peng’s team at Palleon has created a means to produce the antibody-enzyme combo without a tricky chemical synthesis. All they have to do is take an existing tumor-targeting antibody and hook it onto the enzyme, says Jason Luke, a medical oncologist at the University of Chicago School of Medicine, who leads a Palleon-funded research project to see if glycan-modifying enzymes correlate with clinical outcomes. “This is about as straightforward a drug development program as you could want. It’s translatable to other surface proteins, and they could easily make additional therapies.”
Whereas the vast majority of immune therapies target a single molecular interaction, Bertozzi’s is a broader approach that is “much more robust because sialic acids are recognized by multiple receptors on different immune cells,” says Yvette van Kooyk, an immunologist at VU University Medical Center in the Netherlands, who wrote a recent review about cancer’s “glyco-code” and learned about Palleon’s drug program at an earlier cancer conference in September 2018. The cancer field has really neglected the importance of glycans,” van Kooyk says. “But they have a very immune-suppressing function. To overcome that, it’s necessary for new treatments to also do something with these glyco-codes.”
Note: This article was updated after it was initially posted.