Editor's Note (9/29/20): This story has been updated and republished in light of the Trump administration’s newly announced plans to ship millions of antigen tests to states and vulnerable communities.
An inexpensive coronavirus test that millions of Americans could use at a pharmacy, in a workplace or even at home could prove to be a vital asset in allowing people to return to jobs and school. Deborah Birx, the White House’s coronavirus-response coordinator, has called rapid antigen tests the “breakthrough innovation” that is needed to perform hundreds of millions of such assays a day. The remarks echoed her previous statements that antigen tests might be used to examine broad swaths of the public.
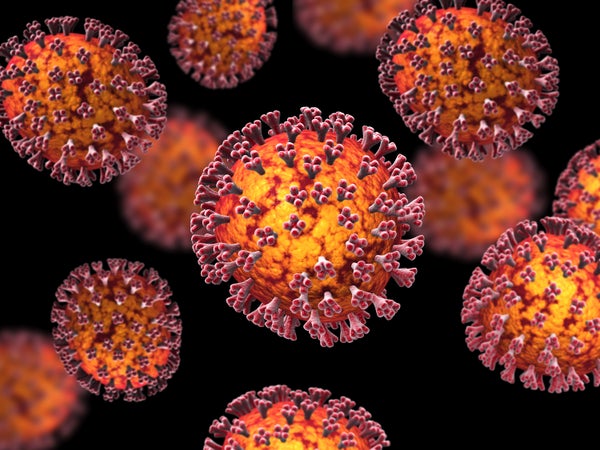
The technique often involves a technology—called a lateral flow assay—similar to that employed in home pregnancy tests. In the test, an antibody can bind to one of the spike proteins (the antigens) that cover the surface of the virus like the spines on a puffer fish. The tests are inexpensive to produce and simple to use, and they deliver results in minutes. On September 28, several months after this story was originally published, the Trump administration announced a plan to distribute 150 million of these assays, developed by Abbott Laboratories. The test, called BinaxNOW, correctly identifies 97.1 percent of positive cases and 98.5 percent of negative cases, and it provides results in 15 minutes. An Abbott spokesperson declined to comment on the record about the test’s accuracy.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The goal is also to field a test that is just as accurate as the current standard, which uses polymerase chain reaction (PCR) to process the virus’s genetic material and amplify it for detection. But major technical hurdles still remain. “What you would want in terms of a breakthrough is that [an antigen] test is more sensitive, [or less prone to false negatives], and easier to use than a PCR-based test. And that is not so easy to do,” says Bettina Fries, chief of the infectious diseases division at Stony Brook Medicine. “Normally, PCR-based tests are more sensitive.”
The urgent need to conduct massive levels of testing means that any feasible technology is being considered. OraSure Technologies, a medical device company in Bethlehem, Pa., received a $710,310 federal contract last month for an in-home assay that can potentially detect a coronavirus antigen in saliva in as little as 20 minutes. Stephen Tang, the company’s CEO, says such antigen tests are needed to screen millions of people per day. “You can’t be dependent on the throughput of laboratories and the availability of medical and laboratory professionals,” as PCR assays typically require, to conduct widespread testing, he says.
Because a PCR test makes thousands of copies of its target RNA, it is able to detect a virus at far lower concentrations, called the limit of detection, than antigen tests typically can. PCR’s limits of detection “are on the order of a few hundred virus particles in a milliliter of transport liquid,” says Geoffrey Baird, acting chair of laboratory medicine at the University of Washington’s School of Medicine.
In contrast, the sensitivities of rapid antigen tests have been mixed. A 2016 analysis of 116 such tests for the bacteria that cause strep throat, for example, found they had a sensitivity of 86 percent on average—turning in false negative results for 14 percent of people with strep. Antigen tests used to diagnose viral infections such as the flu are even less sensitive, often reporting a negative result when the virus is actually present. Their specificity, or ability to correctly avoid false positive results, is often much higher. They can exceed 95 percent, meaning less than 5 percent of people without infection would test positive.
Birx had said that antigen tests could be used as first-pass screening tools that would be confirmed with follow-up PCR assays. Otto Yang, an infectious disease researcher at the University of California, Los Angeles, is uncertain if that goal can be achieved. “Generally, when you’re doing it that way, you aim for higher sensitivity and less specificity in your screening test,” he says. “It only makes sense if you’re trying to save money or reagents, and you don’t have the capacity [to do PCR]. The only potential benefit would be cost savings, but the loss of sensitivity is a big problem.” The approach would make sense, Yang adds, only if the first-pass screening test was at least as sensitive as PCR in addition to being cheaper.
His view will by no means close the debate on the validity of antigen testing. Lee Gehrke, a microbiologist at the Massachusetts Institute of Technology who co-founded E25Bio, another company developing a coronavirus antigen assay, balks at comparisons of such tests’ accuracy with that of PCR. “The use of the test needs to be tailored to the setting,” he says. “In back-to-work, back-to-school settings, repeated, regular testing is going to be needed. If the testing is repeated, I believe the rapid [antigen] test will pick [the virus] up.”
Gehrke acknowledges that infected individuals can have viral proteins present at levels below the test’s limit of detection in the first few days of infection. He says those levels will increase as the infection progresses, however. “It’s possible that at the very left end of that bell curve, there’s a time that PCR can detect [the virus] but the rapid antigen test doesn’t,” Gehrke says. But if the goal of testing is to get people back to work, he adds, a test that has “less than perfect” sensitivity will be acceptable if it is also inexpensive.
Yang counters that antigen tests could find a place as a diagnostic tool, yet the results they provide may be unable to serve as a much needed early warning signal. “If your goal is to detect somebody that has a virus that may be more contagious [with a greater volume of the pathogen], then maybe that does make sense,” he says. But if the objective of a periodic antigen test is to detect people early in infection, “there will be less virus, and so sensitivity will be a big issue.”
The acute need for this type of testing, however, will continue to provide momentum to this line of research. “Rapid tests are going to miss people who are sick, but they are still very valuable, because they take just a few minutes to test somebody,” says Gigi Gronvall, an immunologist at the Johns Hopkins Center for Health Security. “If we’re able to scale up PCR, that will give you a more accurate, sensitive result. But there is some value at the point of care to having a screen like this.”
Ultimately, these debates may be put to rest in a few years. “Getting testing broadly is clearly something that we need to contain the epidemic. But all of this is a stopgap,” says Karla Satchell, a microbiologist at the Northwestern University Feinberg School of Medicine. “What we really need is a vaccine.”
Read more about the coronavirus outbreak from Scientific American here, and read coverage from our international network of magazines here.