Some half a million people worldwide with severe hearing loss use an electronic implant in the ears to be able to let them understand speech. Cochlear implants, as they are known, are one of the most successful technologies to have come out of neuroscience, but only provide partial correction for any hearing deficit. They are not a bionic device that lets people enjoy a Mozart symphony or make out a friend’s gossip in the din of an outing at a local club. “If they go to a restaurant, it’s very hard for them to understand speech,” says auditory neuroscientist Tobias Moser of the University of Goettingen in Germany. “They also suffer from not appreciating melodies.”
Cochlear implants have a maximum of 22 channels to perceive the frequency of an utterance. New research led by Moser has the potential to overcome these limitations by using light to precisely stimulate auditory neurons in the inner ear. Moser hopes the approach may one day improve the current generation of cochlear implants and make speech in noisy environments comprehensible for deaf people.
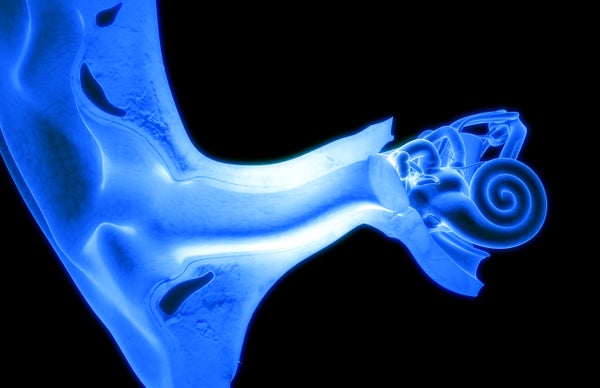
The cochlea is a spiral structure in the inner ear that analyzes sound frequencies. Running through it is a membrane that vibrates in different places in response to the diverse frequencies found in spoken language. The vibrations activate nearby “hair” cells that, in turn, stimulate auditory neurons, sending frequency information up the auditory nerve to the brain.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Sensorineural hearing loss involves loss of hair cells and cochlear implants to bypass the damage by stimulating the neurons directly with electrodes. But current from the electrodes does not move in a direct line from the electrode to an auditory neuron. It tends to diffuse when crossing the tiny gap, causing “cross-talk” with any neighboring electrode placed too closely. As a result, the devices are designed to constrain the number of electrodes to avoid interference, which also limits the number of frequencies that can be discriminated.
The new study, published recently in Science Translational Medicine, uses a technology called optogenetics that replaces electricity with light. “Average performance with cochlear implants has plateaued over the past decade, so everyone’s looking for that next step,” says otologist Daniel Lee of Harvard Medical School, who was not involved in the study. “Optogenetics is a reasonable solution, because you can focus [light] and steer it in a way you really can’t do with electrical stimulation.” Optogenetics, a widely used research technique in animal studies, involves introducing genes that produce light-sensitive proteins (channelrhodopsins, or “opsins”), into neurons, allowing them to be activated with light.
Moser’s group published a study in 2014, using rodents engineered to express opsins from birth. The new study used gerbils, which can hear the lower frequencies that humans perceive. The researchers’ genetic manipulation was in adults and used a faster opsin (one that recovers quicker between activations) to improve the system’s ability to reproduce precise timing information in sounds. They injected a virus into the gerbils’ cochlea, which carried the opsin gene into the auditory neurons. They then used an optical fiber to beam light into the cochlea through a hole in the round window (a small opening between the middle and inner ear). This produced responses in the gerbils’ auditory brainstem that were similar to those evoked by sound, and which remained stable over a period of weeks.
To test the system, the team trained gerbils to avoid a shock by jumping a barrier upon hearing an alarm. They first trained normally hearing animals using light, showing that optical stimulation influenced behavior. They then showed that animals trained using light also jumped in response to sound. “This doesn’t say it sounded exactly the same, but it was sufficiently similar,” Moser says. Finally, they deafened a group of gerbils with a chemical, then showed that although they no longer responded to sound, the animals quickly learned to use light stimulation instead, showing that some auditory function was restored in the deaf animals. “These are impressive results, showing a credible new means of restoring activity to the deaf auditory system,” says neuroscientist John Middlebrooks, of the University of California, Irvine, who was not involved in the work. “With substantial future research effort there’s potential to move ahead of [beyond] what can be accomplished with a cochlear implant.”
The study used only a single optical channel and so could not measure frequency resolution—an important next step will be developing multi-channel devices. Options for device design include micro-LED arrays and “wave-guide” technology that can steer light from optical fibers. Fiber-optics consume a lot of power though, leading to devices of unwieldy size. “LEDs are better, but dimmer, so there are some technological challenges,” Lee says. “Things will improve, especially as more opsins become available that have lower thresholds.”
Other hurdles remain before the approach could be used in humans. But although virus-induced genetic manipulation is generally not done in humans, the ears (and eyes) are good candidates for such methods, as they are both less strictly guarded by the immune system and more anatomically isolated so that the inserted gene stays in its intended place. All of this presents its own challenges, as the cochlea is so isolated (it’s encapsulated in a bony shell) it is difficult to access. The team found that less than half of injected animals showed responses to light, less than a third of neurons incorporated the protein, and around a quarter of neurons were lost, presumably due to damage from the injection. On the bright side, neurons along the cochlea spiral expressed the gene that produced the opsin protein. The team did not detect that other cells besides the auditory neurons incorporated the gene. The researchers plan to start trials in non-human primates this year, which have more similar immune systems to us, and use vocalizations that will be useful for comparing performance between devices. “We will probably know in about two years whether we feel comfortable translating this into a medical device,” Moser says. “So far things look pretty good, but there’s a long way to go.” He has started a company named OptoGenTech, which launches next January, to help commercialize the technology.