When glial cells were discovered in the 1800s, they were thought to be passive, supporting structures—the “glue”—as their Greek name implies—that holds neurons together in the brain and throughout the nervous system. In recent years, however, neuroscientists have discovered that far from being passive, these small cells play an astonishing variety of roles in both the development and functioning of the brain. Some of the latest discoveries suggest that glia play complex roles in regulating appetite and metabolism, making them a possible target for treating obesity.
Signs that glia might play such roles were first identified in the 1980s. Neuroscientist Pierre Magistretti and his colleagues found evidence that neurotransmitters could promote the release of glucose reserves stored in astrocytes, a star-shaped type of glial cell. Otherstudies revealed that obesity leads to increased activation of glial cells in the hypothalamus—the key area of the brain for controlling metabolic processes. This was despite the fact that, for a long time, “neurons were considered the only players in the control of energy metabolism,” says Cristina García-Cáceres, a neurobiologist at the Helmholtz Diabetes Center in Germany.
Glia and glucose
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Two recent studies add new evidence that glia play a key role in metabolism. In one study, published last week in Cell, García-Cáceres, together with Matthias Tschöp, the director of the Helmholtz Diabetes Center and colleagues, reported that insulin acts on astrocytes to regulate sugar intake in the brain.
The researchers used genetic engineering to remove insulin receptors from astrocytes in adult mice. Then, using positron emission tomography imaging, they discovered that these mice did not have enough glucose reaching their brains. As a result, the mice were unable to adjust the amount they ate to balance the sugar level in their bodies. They also displayed reduced activity in specialized brain cells called proopiomelanocortin neurons, which are involved in signaling satiety.
In a subsequent experiment, the researchers discovered that if they removed the receptors for both insulin and leptin, a hormone released by fat cells that regulates eating behavior, from the animals’ astrocytes, the mice developed pathologically high sugar levels in their blood. The findings suggest that these hormones work together to regulate metabolism.
“[The researchers] show that these manipulations have a clear physiological effect on glucose metabolism,” says Magistretti, who was not involved in either study and is currently on the faculty of Switzerland’s École Polytechnique Fédérale de Lausanne and the King Abdullah University of Science and Technology in Saudi Arabia. “It's extremely elegant and precise.”
To divide and protect
Around the same time, another group of researchers led by Maia Kokoeva at McGill University in Canada was investigating a different type of glial cell—NG2-glia, or oligodendrocyte precursors. In previous studies, Kokoeva and her colleagues found that the majority of cells dividing in the hypothalamus—a whopping 80 percent—were NG2-glia, which sparked their interest in finding out why the cells were so abundant.
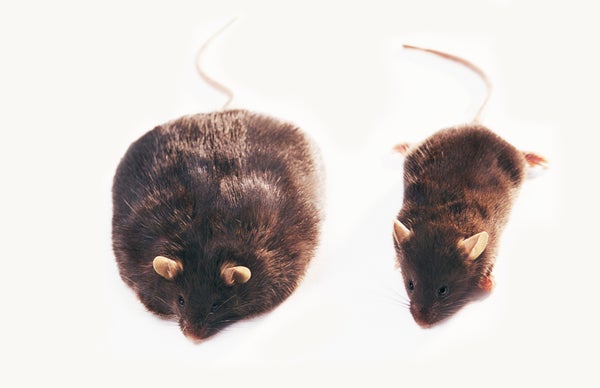
To answer this question, they blocked the proliferation of NG2-glia in mice and found that without them neurons in the arcuate nucleus, a structure near the base of the hypothalamus, became unresponsive to leptin. This caused the animals to overeat, leading some to double in weight in just a month. “[One thing] we are interested in next is to understand the mechanism of the interaction between the leptin receptor neurons and the NG2-glia,” Kokoeva says. The study appeared in May in Cell Metabolism.
“Here, two groups independently [observed] that the cells that are key in sensing the status of the periphery and responding appropriately are not neurons like everybody would think, but glial cells that then have an effect on neurons,” Magistretti says.
Future obesity treatments
When Jeffrey Friedman and his group at Rockefeller University first discovered leptin in 1994, it seemed like the long-sought solution to obesity had finally appeared. However, the reality turned out to be much more complicated. “We now know that there are dozens, if not hundreds, of hormones and signals regulating not only glucose metabolism but energy metabolism, food intake and lipid metabolism,” Tschöp says. “And that's all interlinked in a very, very complex system.”
Despite major advances in understanding how neurons control the body’s metabolic processes, scientists are still far from finding a cure for obesity, which has reached pandemic levels in many countries. Researchers investigating glia hope that focusing on these long-overlooked cells will provide some much-needed advances. “By looking at the bigger picture of what hormones and metabolites do to different types of cells in the brain, we may be able to tailor novel preventive and therapeutic approaches that will allow us to turn around [the] pandemic,” Tschöp says.