Neurodegenerative diseases all involve the accumulation of toxic versions of naturally produced proteins in the brain. Multiple proteins are often abnormal in a patient, and the same aberrant protein can be involved in several different conditions. One common culprit is tau, which is abnormal in various conditions: chronic traumatic encephalopathy, a neurodegenerative disorder caused by repeated head trauma; a group of conditions known collectively as frontotemporal dementia; and, most famously, Alzheimer’s disease (AD).
Normally, tau stabilizes structures inside neural connections, called microtubules, which facilitate chemical communication between cells. In disease states, tau is chemically altered, becoming misshapen and breaking away from microtubules. These toxic versions accumulate into structures called “neurofibrillary tangles,” which disrupt cells’ ability to communicate and may trigger other forms of damage, such as inflammation. Tau is involved in AD, but abnormalities in a different protein, amyloid-beta, are thought to be the initial trigger for a chain of biological events (including tau pathology) that underlies neurodegeneration. This is why most AD drugs developed to date have targeted amyloid, although tau has received increasing attention as multiple drugs intended to remove amyloid have failed.
A new study, published Wednesday in Science Translational Medicine, suggests that an existing drug, lonafarnib, could be repurposed to treat neurodegenerative diseases that involve tau. A team of researchers, led by neuroscientist Kenneth Kosik of the University of California, Santa Barbara, found the drug had beneficial effects on tau-related pathology in mice, if administered early over an extended period. They also found evidence suggesting it works via a previously unknown biological mechanism. “This opens up a previously completely unsuspected pathway for tau degradation,” says Kosik, a longtime tau researcher. “We don’t have all the molecular details, but as a place to look, this is full of new opportunities.”
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The last big hope of a major advance for Alzheimer’s being just around the corner effectively died last week, when pharma company Biogen announced it was halting two late-stage clinical trials of an Alzheimer’s treatment, aducanumab. The drug was an antibody aimed at clearing the amyloid “plaques” that are found in the brains of people with Alzheimer’s disease. It had shown promise in early trial results, but, like many before, has fallen at the last hurdle. “Given the setback we've had recently, and many before that, with amyloid, the field is a little bit desperate to find new approaches,” Kosik says. “I think interest in tau is going to go up.”
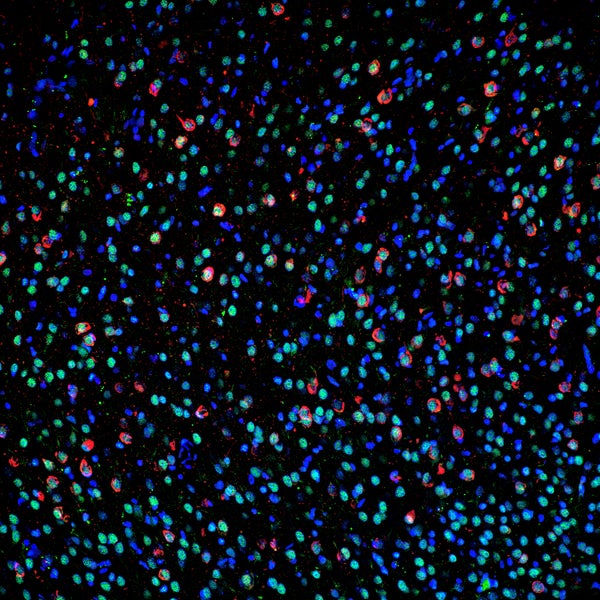
The team first found that lonafarnib lowered abnormal tau in cell cultures, then turned to testing it in mice engineered to possess a mutant version of the human tau gene. These mice, which are commonly used as a model of frontotemporal dementia, start developing tau pathology, brain inflammation and behavioral problems, at around 10 weeks old, and by 20 weeks these problems all reach advanced stages. The researchers began giving the mice lonafarnib at 10 weeks, on an intermittent, five-day-on, five-day-off schedule, then evaluated them at 20 weeks. The treatment markedly reduced abnormal behaviors seen in untreated mice, such as continuously running in circles and a lack of normal nest-building behaviour. “It had rather dramatic effects,” Kosik says. “All the control animals, by 20 weeks, were just really sick, and our [treated mice] were not.” It also reduced tau abnormalities, tangle formation, brain atrophy and inflammation. “We were quite amazed to see there was very minimal deposition of tau tangles,” Kosik says. “And there was reduction, but not elimination, of brain inflammation known as microgliosis”.
The drug appears to work in a fundamentally different way to previous approaches, by activating cellular waste-clearance systems to break down the toxic proteins. Previous strategies have included reducing tau’s production, blocking its aggregation or switching off tau gene expression. These efforts have met with mixed success, but the new findings imply that the cells’ own systems can be recruited to clear pathological forms of tau. “The approach makes a lot of sense,” says neuroscientist Eckhard Mandelkow of the German Center for Neurodegenerative Diseases, who was not involved in the study.
These cleaning-out processes, collectively known as autophagy, deliver cellular debris to a compartment in the cell called the lysosome, which breaks down trash into its component parts for recycling. The team showed that all three known autophagy “routes” were affected by lonafranib, suggesting that the drug may exert its beneficial effects by influencing lysosome activity. Exactly how it does this is not clear, but it seems to involve a protein called Rhes.
Lonafranib blocks an enzyme (called farnesyltransferase) that normally facilitates the activity of a class of proteins, including Rhes, involved in the progression of the cycle of events that lead to cell division. That is why inhibitors of this enzyme—like lonafranib—have been tested as anti-cancer drugs. Why blocking Rhes from interacting with cells should enhance lysosome activity has not been pinned down, but Kosik’s team next wants to probe that question.
The researchers have other reasons to think lonafranib works by influencing Rhes, beyond just noting that it is one of the main targets of the enzyme that the drug blocks. First, when they analyzed which genes were disrupted in stem cell lines derived from people with tau mutations, the RASD2 gene that encodes Rhes turned up. Second, the researchers genetically manipulated Rhes levels in the mice’s brains directly. They found that reducing Rhes reproduced the effects they obtained with lonafranib treatment. This observation suggests the drug lowers Rhes levels, which in turn somehow activates lysosomal activity, which then clears the offending tau molecules. “It’s an intriguing therapeutic hypothesis,” says Larry Refolo, director of Alzheimer ’s disease drug discovery and development at the National Institute on Aging, a department of the National Institutes of Health, who was not involved in the study.
Lonafarnib has been extensively studied in cancer research and was labeled a breakthrough therapy for hepatitis-D by the FDA.* The drug already has a significant safety [profile] in different patient populations, making it attractive for repurposing for the treatment of tauopathies,” Refolo says. An important caveat is that the drug only had these effects when administered early. No benefit was seen in mice whose treatment began at 20 weeks. “It delays the onset, but does not reverse the pathology,” Mandelkow says. “However, this would be a major step, since a significant delay would enable patients to extend their meaningful life, a goal that has long been on the agenda of NIH.”
An intriguing possibility relates to the fact that the team found lowered, not raised, levels of Rhes in the human stem cell lines with mutant tau. “The reason we think it went down is these cells were detecting aberrant tau and self-regulating to lower Rhes levels as a means to activate autophagy and remove the aberrant proteins,” Kosik says. “Rhes seems to be modulating tau levels until its ability to do so is overcome.” The implication is that cells can sense even very low levels of abnormal tau. “If we’re right,” he adds, “the lysosomal system may even be detecting single molecules of aberrant tau and turning on a system to wipe them out.” If that thesis is correct, understanding how this process works might be lead to a new means for early detection and treatment of Alzheimer’s.
Kosik argues that the detailed cell biology implicated by this research should be fully explored before ploughing on with clinical trials targeting tau. The leading approach at the moment is targeting tau with antibodies. “I really hope the tau people don’t make the same mistake the amyloid people have, by using a lot of tau antibody trials before we truly understand whether they’re engaging the correct target,” Kosik says. “We didn’t know that for amyloid, and we don’t know that for tau.”
Tau can take several forms, and geneticist Michel Goedert’s group at Cambridge University in the U.K., recently published evidence that different forms are specific to different conditions. Tau also exists in soluble (liquid) and insoluble forms (solid precipitates). “We don’t even know what the toxic form is yet,” Kosik says. Furthermore, researchers don’t yet know if antibodies can actually access the offending molecules, even if the right ones are identified. “There’s many reasons why we don’t have enough knowledge to invest hundreds of millions of dollars into tau antibody trials,” Kosik says. “And go through the same demoralization we have with amyloid.”
*Editor’s Note (3/28): This story was edited after posting. It incorrectly stated that lonafarnib had been approved for hepatitis-D but was not in use.