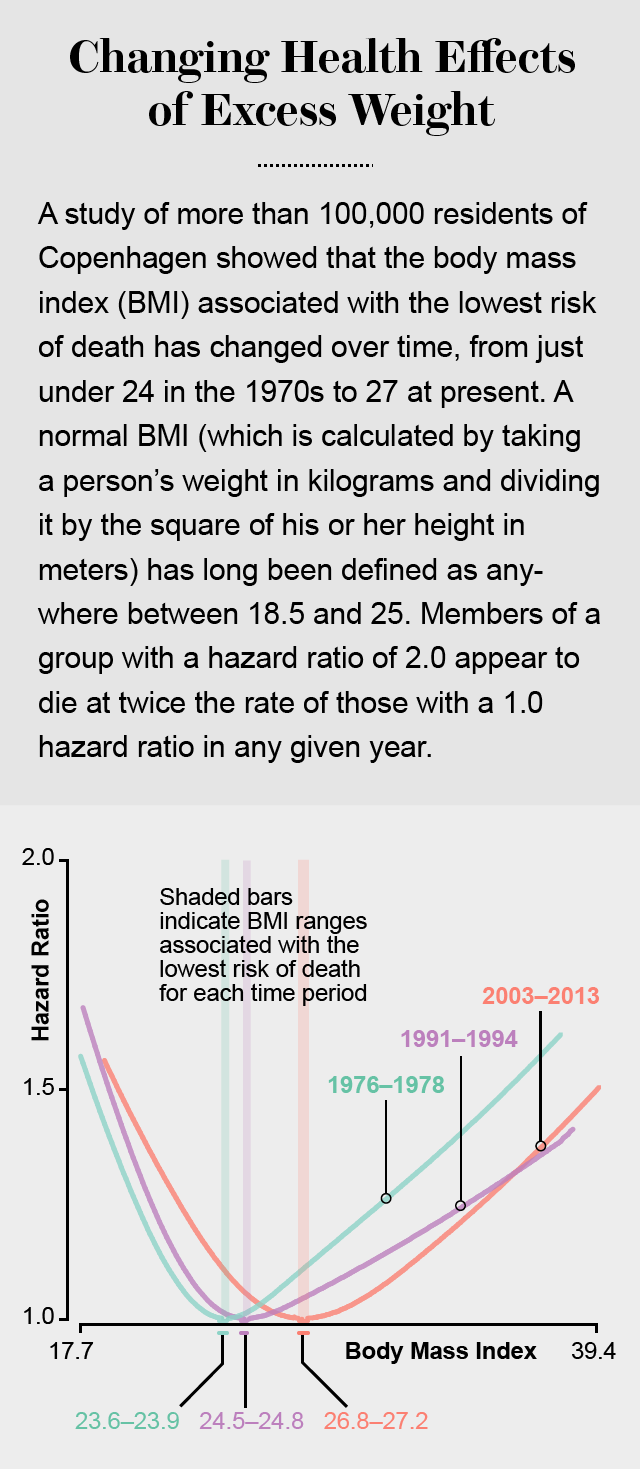
People who are slightly overweight but not obese—as defined by their body mass index (BMI)— tend to live longer than their normal-weight counterparts, according to a new Danish study. But that has not always been the case. In the 1970s, the Danish data show, study subjects with the best chance of living longer tended to have a BMI in the normal range, defined as being between 18.5 and 25. Someone who is 1.65 meters (five feet, four inches) tall and weighs 68 kilograms (150 pounds) would have a BMI of 25.
At the extremes—of severe underweight or obesity—the Danish data show an increased risk of dying from all causes, particularly cardiovascular disease. The cutoff for considering whether someone is obese may be different, however, for different races and ethnicities. (All the Danes studied were white.) Asians from the Indian subcontinent are a case in point. South Asians tend to have more body fat for the same BMI compared with other groups. So the deleterious effects associated with weight gain tend to show up at lower absolute weights for them.
The new study may say more than anything else, however, about the health benefits of living in Denmark—all the participants lived in Copenhagen. Virtually all Danes are protected by a universal health care system that takes very good care of residents from the cradle to the grave. It is possible that medical advances over the past few decades in the treatment of type 2 diabetes, hypertension and high cholesterol levels have had a greater impact on people who are overweight—which increases the risk for these conditions—whereas the effect was much smaller in those of normal weight.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Despite this and other caveats, the report, which was published in JAMA The Journal of the American Medical Association, adds to the growing evidence that carrying a little bit of extra weight—especially after midlife—might not be as bad for your health as was once thought. Overall, the BMI associated with the lowest risk of dying from any cause for the Copenhagen cohorts was 23.7 in the 1970s, 24.6 in the 1990s and 27.0 in the present.
A similar upward trend showed up even in people who had never smoked and had no history of heart disease or cancer. For them, the BMI associated with lowest risk of death from all causes crept up from about 18 in the 1970s to 26.1 today.
When the researchers separated the cohorts into two age groups—younger than 60 and older than 60—the BMI that correlated with the lowest risk of death crept up a bit as people got older. In the 1970s, it was 23.5 for those who were 60 and younger and 24.4 for those who were older than 60—both still well within the normal range. From 2003 to 2013, the BMI linked to the lowest mortality was 26.7 for those 60 and younger and 27.3 for those over 60, which is just inside the overweight category.
Source: "Change in Body Mass Index Associated With Lowest Mortality in Denmark, 1976-2013," by Shoaib Afzal, et al in JAMA The Journal of the American Medical Association, Volume 315, No. 18, May 10, 2016.
Graphic by Amanda Montañez
The results echo those of several other large studies that have found that being slightly overweight appears to be protective—especially after middle age. Still, there is no way of concluding that increased weight per se is the protective factor. As with any epidemiological study, even one that is as well-designed as this one, correlation does not prove causation.
“This question has been around for at least 40 years,” says David Allison, an obesity researcher at the University of Alabama at Birmingham (UAB), who was not part of the research. The late Reuben Andres, the first clinical director of the National Institute on Aging in the U.S., brought it up in the 1980s. Katherine Flegal at the National Center for Health Statistics demonstrated the trend in national data in 2005 and international data in 2013. At this point, “it’s almost indisputable that the correlation exists,” Allison says. “What is disputable is what the correlation means.”
Maybe it’s not the weight as such, but just the ability to gain weight that is a mark of health. (Losing weight without wanting to is often a sign of illness.) And so gaining a little extra weight with age is merely a sign of overall health until you end up gaining so much weight that it is unhealthy. In that case, it would be hard to parse the statistics finely enough to show the difference.
Or maybe doctors do not treat people who have normal weight as aggressively as they do those who are overweight.mOr maybe, just maybe, it is simply harder to know what is going on in the border areas between a BMI of 25 and 27. Perhaps, for some people, a little bit of extra weight is protective; for others it isn’t—and researchers really can’t explain why. “These epidemiological studies do not give us an answer,” says Tapan Mehta, a biostatisticianat the UAB, who was not part of the study. “They give us interesting questions to go after.”
And for those of us who want answers now? “What the data clearly show across most ethnicities and races—if you are extremely obese, having treatment will be beneficial,” Mehta says. As for those with just a few extra pounds, it never hurts to eat more fruits and vegetables, get more sleep and exercise and stay tuned.
