Latin America has become the new epicenter of the global COVID-19 pandemic. At a media briefing on June 9 Carissa Etienne, head of the Pan American Health Organization (PAHO), offered a clinical but dire assessment by moving through a chillingly long list that encompasses countries from Mexico to Chile.
“In Mesoamerica, case counts are rising in Mexico, Panama — and in Costa Rica, where we are seeing increased transmission around the Nicaraguan border,” she said. “In South America, the virus continues to spread aggressively in Brazil, Peru and Chile. We’re also seeing, in Venezuela, that cases are now mounting faster than at any point during the country's outbreak. In the Caribbean, cases are on the rise in Haiti. And after more than a month without a new case, Suriname reported a spike this past week.”
In the absence of a vaccine or effective treatments, social distancing measures—primarily stay-at-home orders—are being prescribed, as they have in countries around the world. Similar to other hard-hit regions, there is persistent fear of the virus overwhelming health care systems in Latin America. Yet a number of countries are already planning reopenings—and some never instituted shutdowns at all. To understand how health authorities are negotiating the conflicting demands of the crisis, Scientific American asked Marcos Espinal, director of PAHO’s Department of Communicable Diseases and Health Analysis, to share his perspective.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
[An edited transcript of the interview follows.]
There are more than 1.5 million cases of COVID-19—and more than 70,000 deaths from the disease—in Latin America as a whole. The region has shifted to become the pandemic’s epicenter. What are the projections for infections there going forward?
If you look at different academic institutes worldwide, even the most accurate of them are changing their projections every week. What I can tell you is that June is going to be a tough [month] for Latin America. And [the number of infections] will depend on the mitigation measures that are under implementation [in each country] and how fast they reopen.
We’re not telling anyone don’t open, because that’s a prerogative of every country. But we tell them, “We can accompany you on this,” in the analysis of how to proceed. If they decide to open, it should be by phases. And at the same time, they should have a mechanism that allows them to offer very broad testing in order to continue detecting cases—and a system to do contact tracing and isolation.
Do you believe the number of infections is even higher than reported, given the low levels of testing in some countries?
It is higher, because no country in the world has the real number of cases. Remember, even in rich countries, some people decided not to go and be tested. But it’s clear that the number of cases in Latin America is underestimated.
Are there enough tests available in the region? What is happening in nations, such as Nicaragua and Venezuela, that have had transparency issues in reporting their number of cases?
Well, [the answer] varies. It depends on the approach of each country. Chile is doing 30,000 tests per million people—one of the best [efforts] in terms of testing. Uruguay is doing 13,000 tests per million people. And then Brazil is still slow: we’re still only doing 4,000 tests per million people.
Venezuela and Peru, for instance, are doing a lot of testing but mostly rapid testing. The rapid tests are not good for diagnostics, because they are faulty.
You asked about Nicaragua: Actually, they are not reporting [test results]. There are these rumors that apparently Nicaragua is adopting the “herd immunity” [approach]. But look at what Sweden declared [earlier this month]—that they now regret the number of deaths [after deciding against a lockdown strategy].So basically, the herd immunity approach doesn’t work. [Editor’s Note: Sweden, which initiated only limited distancing measures, has more cases and deaths than other Scandinavian nations.]
More than 190 million Latin Americans, 30 percent of the population, live in poverty. What role does this play in the region’s ability to overcome this pandemic?
How can you demand from a person living in crowded conditions in the belts of Bogotá, Lima, São Paulo, Santo Domingo, Mexico City to practice social distancing if they need to feed two or three kids, and they need to go out?
PAHO is an agency that understands the problems of Latin America. We’re not saying [countries] need to implement 24-hour lockdowns, because we know that we still have barrios, favelas, highly urbanized cities and a highly informal economy in the region [that needs to be maintained for poor areas to survive]. What we tell the countries is be innovative. Some of them are doing curfews at night. Some of them are locking specific barrios or cities.
Given the limitations these countries face in curtailing economic activity, what will be the impact on halting the spread of COVID-19 in the region?
We’ve been seeing countries that are reopening very early, and then they have a [new] peak. The epidemic started in neighborhoods where people were middle- or high-income. The recipe for disaster in this epidemic, which is happening now, is that it has started to reach poor neighborhoods, where there is also the problem of water and sanitation. How can you wash your hands if you don’t have access to water?
Brazil now has the second-largest number of COVID-19 cases in the world after the U.S. And the government of President Jair Bolsonaro has downplayed the seriousness of the pandemic. Is there anything that can be done to slow down infections in the nation?
Brazil is the epicenter indeed. Every virus has its own natural course, and if you don’t implement a package of measures (and we're not talking about only social distancing; we’re talking about PPE, laboratory testing, education to the people), then, definitely, you will suffer. The advantage is that Brazil is a vast country where the [local] governments have the authority to implement measures. And many of them are doing that. But there are some hotspots that are really sensitive now in Rio de Janeiro, São Paulo, Manaus. In some cities in Brazil, in some states, the occupancy rate for beds in ICUs is more than 80 percent.
[How particulates from Brazilian rain forest fires may exacerbate COVID-19 infections]
Why are some countries, such as Uruguay, Paraguay and Costa Rica, having low death and transmission rates while others, such as Brazil, Ecuador, Peru and Panama, are being hit harder by the pandemic?
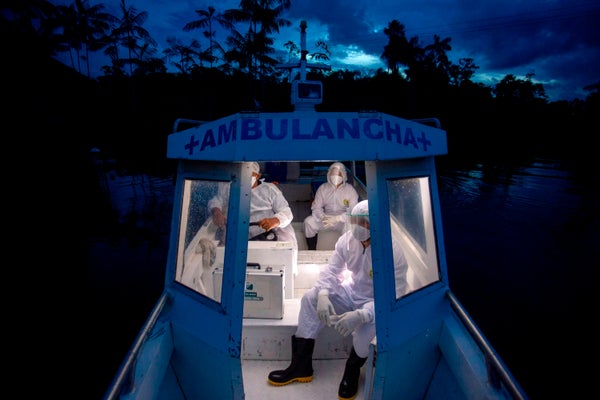
Well, it’s difficult to compare. Some of [these nations] are very big. Some of them are very small. Population is also an issue. The urbanization of the cities is another issue, but it also depends on the intensity with which you implement [a mitigation measures package]. Costa Rica, for instance, uses a very innovative way, with mobile primary health care teams visiting people who are isolated at home. [Editor’s Note: Last week, Costa Rica’s cases peaked in the area of its northern border with Nicaragua. Last Wednesday, the country reported 86 new cases, its highest number since the start of the outbreak. There is still no community contagion, however.]
What is the impact of COVID-19 on other health issues in Latin America? And how does the pandemic exacerbate such existing problems?
The message is: please don’t turn away from other health problems. Latin America and the Caribbean have achieved great strides in reducing morbidity and mortality for infectious diseases. [The Americas were] the first region to eliminate polio. Now we’re seeing an increase in noncommunicable diseases. It’s a dual epidemiological profile in Latin America and the Caribbean, but now [the illnesses that are an issue are] mostly noncommunicable, because of the great work the Americas has done in vaccinating and immunization.
There are about 30 diseases or conditions that we are targeting for elimination between now and 2030. And that is the problem here—and the risk: If we take away our attention to these vital problems, then we will be paying a very deep price, because we will not be able to finish the job. And we need to finish the job.
Are there any diseases, such as dengue, that are being left behind because of COVID-19?
We don’t want to point to any specific disease. But dengue is certainly a huge epidemic, and it has been for the past few years. We have plenty of countries targeted for elimination of malaria. It’s not only about COVID-19. It’s about health, and this is why the message [is the need] to invest in health.
Remdesivir looks like it might have some effectiveness. It is potentially an expensive drug, however. Does PAHO have any plans to facilitate access to remdesivir or similar medications as they come along?
Yes, and [nations] are using it in the region. PAHO has two keys to critical tools: the Revolving Fund for Vaccines Procurement and the Strategic Fund for [the acquisition of] commodities, in which countries advance money, and we can negotiate with different suppliers. PAHO will make sure that countries have access to any new drug or vaccine.
Is there any promising COVID-19 research being done in Latin America?
Some of the countries are participating in the in the World Health Organization’s [WHO’s] Solidarity Trial, where four drugs are being looked at. And there is also a private partnership with academia. So there is no doubt that countries of the Americas are participating in research and development.
How are face masks being used in the region?
The top priorities are for people hospitalized [and] for health care workers that are in the front of the battle. The second priority is for people who are isolated at home and the people who are taking care of these people. Then, if we have extra, they can be used [by the rest of the population].
We’ve already discussed that it’s difficult to maintain a lockdown in Latin America because of the economic situation. So shouldn’t the use of cloth face masks be encouraged by a clear instruction from the WHO rather than just a suggestion?
Look, yes, I agree with you. I think the cautions of the recommendation [from the WHO]is because of the shortages. We don’t want people to start using N95 or N99 respirators and surgical face masks in the streets because we need them to protect the health care workers. But I think we are seeing more and more evidence that [employing masks] doesn’t hurt. And probably the organization will have to issue something. [Editor’s Note: On June 5 the WHO changed its advice on face masks, saying they should be worn in public where social distancing is not possible to help stop the spread of the coronavirus.]
Read more about the coronavirus outbreak from Scientific American here. And read coverage from our international network of magazines here.