When the mystery virus was first detected in Saudi Arabia three years ago, researchers did not know quite what to make of it. The virus causing Middle East respiratory syndrome, or MERS, it turns out, is a cousin of the bug behind severe acute respiratory syndrome (SARS), and has been responsible for the deaths of more than 500 people, primarily in the Arabian Peninsula. Researchers on August 19, however, are reporting that a vaccine has begun to show promise against the disease—at least in monkeys, mice and camels. The vaccine, at both low or high doses, managed to protect monkeys from becoming ill with MERS.
The international team of researchers plans to test whether the vaccine will also prove effective in humans. Even without that assurance, however, the researchers hope that if the experimental vaccine were deployed during an outbreak, it could tamp down disease in camels and potentially break the chain of transmission to humans. “I think this result is very exciting. I was very impressed they looked in diverse animals,” says Trish Perl, an infection control expert from Johns Hopkins University who has worked to help contain MERS in Saudi Arabia. Perl was not involved in this new research, published in Science Translational Medicine.
The new vaccine, injected multiple times five weeks before exposure to the virus, protected eight rhesus macaques from developing the disease. Four nonimmunized monkeys, meanwhile, became infected and became sick. The experimental vaccine also prompted mice and three inoculated camels to develop antibodies against the virus. (The research team did not go on to expose the vaccinated camels to live virus like they did with the monkeys because camels are so large and the researchers did not have access to a specialized facility to safely contain the infected creatures.) “The camel [antibody] data is very exciting to us,” says senior author David Weiner, a professor of pathology and laboratory medicine at the University of Pennsylvania Perelman School of Medicine. Most researchers believe that humans contract the disease through close interactions with camels. “The camel is a reservoir for this disease and we believe it’s the juvenile camels in particular that don’t appear to have strong immunity to MERS,” Weiner says. “So the vaccine could be used in that population.” (The camels used in this study were not juveniles.)
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Without any vaccine or cure to combat the virus it has managed to spread among more than 1,400 people in the past few years. Most cases among humans have been in the Middle East although there was an outbreak in South Korea this year after an ill traveler returned to Seoul from the Middle East. For unknown reasons, the number of human infections surges in the springtime.
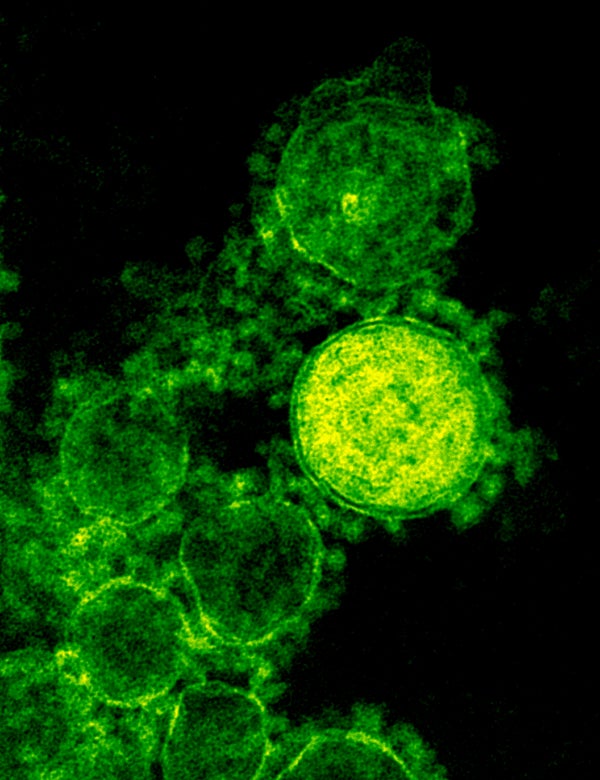
MERS is caused by a coronavirus—named after the hallmark “crown” that appears on the viral protein’s outer shell. The virus, which most experts suspect is carried in bats as well as camels and only rarely makes it into humans, is transmitted from person to person when people come in close proximity to patients ill with MERS and breathe in large amounts of virus. Exactly how the pathogen originally hops from animals to humans remains unclear but virus experts suggest that drinking camel milk or exposure to camel secretions may be the culprits. Humans with MERS typically die from high fevers and pneumonia but patients are most likely to succumb when they have other underlying health issues. “Until the [MERS] problem is addressed at the source—the camel population in the Middle East—we will continue to see community acquired human cases,” says Peter Ben Embarek, the World Health Organization’s point person for MERS. “The Korea event and the ongoing outbreak in the National Guard hospital in Riyadh are examples of how bad it can [become] if cases are not detected promptly and managed,” he said, via e-mail. Saudi Arabia has had almost 50 cases of MERS since the beginning of this month.
Only studies in humans will be able to determine how long the vaccine would last or how many booster shots would be necessary to prevent disease. The team’s new vaccine is not based on a live virus so it is not capable of causing disease or replicating in the body. It has been synthesized by stringing together a short chain of amino acids that mimic a site on the surface of the MERS protein. The introduction of those amino acids into the bloodstream fools the body into thinking it’s under attack and triggers the rise of antibodies.
Delivery of the vaccine requires more than a simple jab. When the inoculation is injected into the body, it is delivered with an accompanying electrical jolt that is intended to spark a more efficient response to the vaccine. The small shock opens pores in cells for milliseconds, allowing large molecules like DNA to travel inward more efficiently. Whether or not patients would be willing to tolerate a potentially painful electric shock for a preventative vaccine, however, remains to be explored.