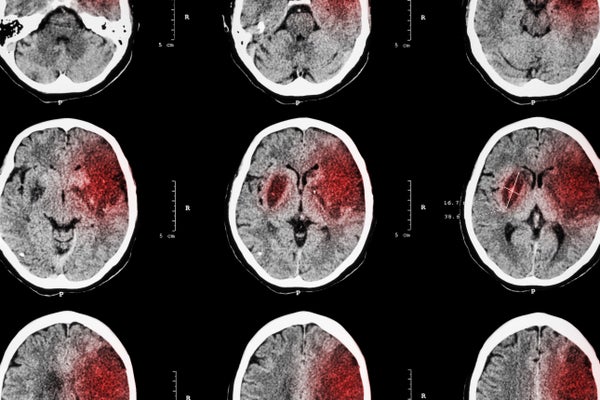
The pathology of a stroke is deceptively complicated. In the simplest sense, strokes occur when the blood supply to a particular region of the brain is interrupted, cutting off the area to oxygen and nutrients. This deprivation results in injury and death to the local brain cells.
But for days after the breach in blood flow, the immune system also does its own fair share of damage to the already injured brain through an inflammatory response. New research by a group at Stanford University has identified a subset of immune cells that drive brain injury following a stroke, raising the possibility that immune-system inhibition might be a promising treatment for a blood-deprived brain. More surprising is that much of the immune reaction to a stroke appears to begin in the gut, shedding new light on our ever evolving understanding of the gut-brain axis. The research was published on July 1 in Nature Immunology.
Strokes manifest in two ways: either an artery in the brain bursts—causing a hemorrhagic stroke—or it becomes clogged, typically by a blood clot, causing the far more common ischemic stroke. In the new study, the authors used positron-emission tomography to scan immune system activity in mice that had the blood in a single cerebral artery interrupted for 45 minutes, mimicking an ischemic stroke.
Specifically, the study looked for increased activation of myeloid cells, immune system “first responders,” as they are sometimes called. Myeloid cell surfaces bear a molecule called TREM1, or triggering receptor expressed on myeloid cells 1, that amplifies immune responses. Normally TREM1 drives the immune system to fight infections, but when it is too aggressive, it can contribute not just to stroke but to other serious conditions, such as heart disease and cancer.
Shortly after experiencing an artificially induced stroke, the study mice had elevated TREM1 levels in the myeloid cells in their bloodstream and spleen, where many immune cells are housed. Within one to two days of a stroke, these TREM1-enriched cells had bombarded the affected area of the brain. It seemed that overexcited TREM1 was contributing to the brain damage. A follow-up experiment provided further confirmation.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
When mice in which the TREM1 gene had been deleted were subjected to a stroke, they had significantly less damage to their brains and exhibited higher survival rates. Mice lacking TREM1 were swifter on their feet and better able to rear up on their hind legs.
Perhaps more striking, a stroke also ignited immune activity in the gastrointestinal tracts of the affected mice. When we—or mice—suffer a stroke, the sympathetic nervous system, which largely lies outside the brain and spinal cord, fires off a signal to the gut that loosens its normally tight lining. Bacteria can then migrate through the intestinal wall, stimulating myeloid cells and also increasing the risk of poststroke infections. The researchers found that after a stroke, TREM1 levels on the surfaces of myeloid cells called macrophages also rose, exposing the body and brain to yet more inflammation.
“The immune, or inflammatory, response is turning out to be a real common denominator among many neurologic diseases,” says senior study co-author Katrin Andreasson, a professor of neurology at Stanford. “The question we asked was: What immunological pathways are involved after stroke? We think we found one.”
Much of the ongoing research in Andreasson’s lab is focused on understanding the interface between the immune system and the brain, particularly in neurological disorders, including not just stroke but also Alzheimer’s disease. She points to the abysmal treatment rates in stroke, with a minority of patients getting the right treatment in the right time frame. “We wanted to look at whether we could modulate the immune response and get a better outcome in stroke,” she says.
“I find the study novel and in line with the emerging idea that systemic factors exert a powerful influence on the way the brain reacts to injury,” comments Costantino Iadecola, director of the Feil Family Brain & Mind Research Institute at Weill Cornell Medicine. Iadecola was not involved in Andreasson’s study but nods to its significance. “Much of stroke research up to the 1990s focused exclusively on neurons, often in a culture dish,” he says. “But now we know that the entire body reacts to brain injury and that peripheral organ systems contribute to the evolution of the brain damage."
Andreasson and her colleagues, including study co-author and Stanford postdoctoral fellow Qingkun Liu were able to reproduce their results by administering part of a protein called LP17, a component of TREM1. LP17 served as a decoy, throwing off the molecular targets that normally increase TREM1 gene expression. In mice given LP17 after blood flow to their brain returned, there was notably less damage—and a diminished presence of myeloid cells. Stroke-affected areas of the brain were smaller by more than half as compared with those in mice treated with a placebo. What’s more, LP17 injections as far out as 48 hours appeared to improve movement and neurological function in subsequent days.
Currently, stroke is treated with drugs that dissolve culprit clots or with clot-removal surgery. Both approaches can be very effective, but as Andreasson points out, only a subset of patients are eligible to receive them, and many get treatment too late for it to be effective. “The deleterious immune activity we’ve focused on in this study goes on for days and may be a new target,” Andreasson says.
“The dramatic protection that TREM1 inhibition exerts on brain and gut raises the possibility that ‘turning down the gain’ of the immune system may be beneficial in stroke,” Iadecola adds. “It would be appropriate for patients in whom [existing] therapies are not indicated, or the majority of stroke patients at the present time.” He also notes that if TREM1 inhibition prevents increased permeability of the gut following a stroke, individuals would be at lower risk for infection, a major cause of death.
Andreasson is planning to continue this line of research, testing how far out TREM1-inhibition therapy can go. She and her colleagues also hope to test the same immune pathways in humans before too long.
“We’ve got a lot to do,” she says. “I’m writing my grant applications right now!”