Humans and other mammals react to stressful situations through a series of well-orchestrated evolutionary adaptations. When faced with a predator looking for its next meal, or with worry of losing a job, our bodies release a cascade of stress hormones. Our heart rate spikes, breath quickens, muscles tense up and beads of sweat appear.
This so-called “fight-or-flight” response served our ancestors well, but its continual activation in our modern-day lives comes with a cost. Scientists are starting to realize stress often exacerbates several diseases, including depression, diabetes, cardiovascular disease, HIV/AIDS and asthma. One theory is hoping to explain the link between stress and such widespread havoc by laying the blame on an unexpected source—the microscopic powerhouses inside each cell.
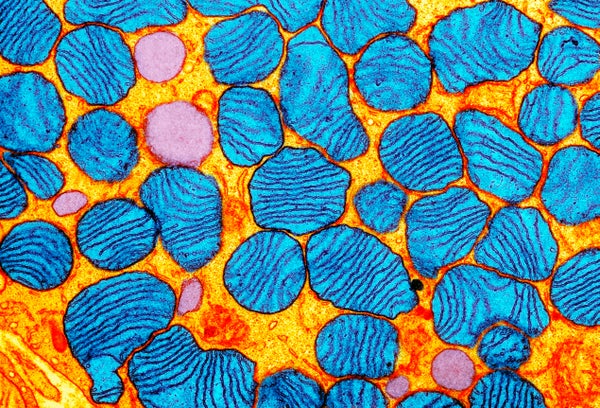
Each of our cells contains hundreds of small bean-shaped mitochondria — subcellular structures, or organelles, that provide the energy needed for normal functioning. Mitochondria have their own circular genome with 37 genes. We inherit this mitochondrial DNA only from our mothers, so the makeup of the DNA’s code stays relatively consistent from one generation to the next.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
But our fight-or-flight response places extreme demands on the mitochondria. All of a sudden, they need to produce much more energy to fuel a faster heartbeat, expanding lungs and tensing muscles, which leaves them vulnerable to damage. Unlike DNA in the cell’s nucleus, though, mitochondria have limited repair mechanisms. And recent animal studies have shown chronic stress not only leads to mitochondrial damage in brain regions such as the hippocampus, hypothalamus and cortex, it also results in mitochondria releasing their DNA into the cell cytoplasm, and eventually into the blood.
The genetic cast-offs are not just inert cellular waste. “This circulating mitochondrial DNA acts like a hormone,” says Martin Picard, a psychobiologist at Columbia University, who has been studying mitochondrial behavior and the cell-free mitochondrial DNA for the better part of the last decade. Ejection of mitochondrial DNA from the cell mimics somewhat adrenal glands’ release of cortisol in response to stress, he says. Certain cells produce the circulating mitochondrial DNA and, as with the adrenal glands, its release is also triggered by stress.
To demonstrate psychological stress can cause mitochondrial DNA to be released by cells, Picard and his team devised a quick stress test. They asked 50 otherwise healthy men and women to deliver a quick speech defending themselves against a false accusation on camera. Afterward the researchers took blood samples from the participants and compared them with blood taken immediately before they were stressed. Even though the stressful task only lasted a total of five minutes, the scientists found participants’ serum circulating mitochondrial DNA levels more than doubled 30 minutes after the test. These results, currently under review, provide the first direct evidence for how bits of mitochondrial DNA floating in our blood may relay stress to other parts of the body, like dominoes tumbling one after another.
Previous studies have provided several clues that suggest circulating mitochondrial DNA is a hallmark of stress. In 2016 Swedish researchers published findings in Translational Psychiatry demonstrating elevated levels of mitochondrial DNA outside the cell in 37 people who had recently attempted suicide. Earlier this year the same group of scientists published another paper inNeuropsychopharmacology showing people with major depression had high levels of circulating mitochondrial DNA, and these levels kept increasing in patients who did not respond well to antidepressant medication.
These studies are all part of an emerging field of research on mitochondrial DNA, where scientists are recognizing that the tiny organelles have effects across a wide range of diseases. “Mitochondrial DNA is probably the most sensitive thing in your body,” says Douglas Wallace, director of the Center for Mitochondrial and Epigenomic Medicine at The Children’s Hospital of Philadelphia. “If your mitochondria are sensing a problem, then all the rest of you is in trouble, too.”
In his own research Wallace has shown mitochondrial DNA mutations are more common in people with autism spectrum disorders than in neurotypical adults. Other studies in the past few years have linked mitochondrial dysfunction to schizophrenia, Alzheimer’s, arthritis and cancer—all problems where inflammation is also known to occur, Picard notes.
But how was this inflammation triggered by mitochondrial DNA leaking out of cells? A 2010 Nature paper provided the answer: In it researchers demonstrated the way mitochondrial DNA, when released into the blood after an injury, mobilized a pro-inflammatory immune response. Because of mitochondria’s bacterial origin and its circular DNA structure, immune cells think it’s a foreign invader. When circulating mitochondrial DNA binds to a particular receptor, TLR9, on immune cells, they respond as if they were reacting to a foreign invader such as a flu virus or an infected wound. The immune cells release chemicals called cytokines telling other white blood cells they need to report for duty at sites of infection, inflammation or trauma.
Together, this growing understanding of circulating mitochondrial DNA sets a time frame for how psychological stress may lead to widespread inflammation, Picard says. “Mitochondria are the missing link between our psychological state and neurological or other disorders involving inflammation,” he says.
It is an interesting shift away from the traditional, anatomical aspects of disease, such as brain shrinkage in depressed patients. But reducing disorders like depression to brain imbalances or shrinkage simply has not explained everything, says Bruce McEwen, a neuroendocrinologist at The Rockefeller University. “If that was the case, you could take Prozac or [selective] serotonin reuptake inhibitors [SSRIs] to fix it, but everybody is now realizing that that’s not the way it works,” he says. “Otherwise, antidepressants would be more effective.”
If further evidence of the importance of healthy mitochondria continues to emerge, drugs that focus on regulating cellular energy production instead could become a new line of defense for psychiatric and biological disorders.