Amid gloomy reports of an impending epidemic of Alzheimer’s and other dementias, emerging research offers a promising twist. Recent studies in North America, the U.K. and Europe suggest that dementia risk among seniors in some high-income countries has dropped steadily over the past 25 years. If the trend is driven by midlife factors such as building “brain reserve” and maintaining heart health, as some experts suspect, this could lend credence to staying mentally engaged and taking cholesterol-lowering drugs as preventive measures.
At first glance, the overall message seems somewhat confusing. Higher life expectancy and falling birth rates are driving up the global elderly population. “And if there are more 85-year-olds, it’s almost certain there will be more cases of age-related diseases,” says Ken Langa, professor of internal medicine at the University of Michigan. According to the World Alzheimer Report 2015 (pdf), 46.8 million people around the globe suffered from dementia last year, and that number is expected to double every 20 years.
Looking more closely, though, new epidemiological studies reveal a surprisingly hopeful trend. Analyses conducted over the last decade in the U.S., Canada, England, the Netherlands, Sweden and Denmark suggest that “a 75- to 85-year-old has a lower risk of having Alzheimer’s today than 15 or 20 years ago,” says Langa, who discussed the research on falling dementia rates in a 2015 Alzheimer’s Research & Therapy commentary (pdf).
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Some of the clearest evidence comes from the Cognitive Function and Aging Study (CFAS), led by Carol Brayne, professor of public health medicine at the University of Cambridge. This study surveyed adults in the U.K. 65 or older in Cambridgeshire, Newcastle and Nottingham in the 1990s and again around 2010. During that period, dementia rates in the older population fell 24 percent—from 8.3 to 6.5 percent. Put another way: if the frequency of dementia in seniors had stayed the same across that period, there should have been 214,000 additional people with dementia than the 670,000 documented.
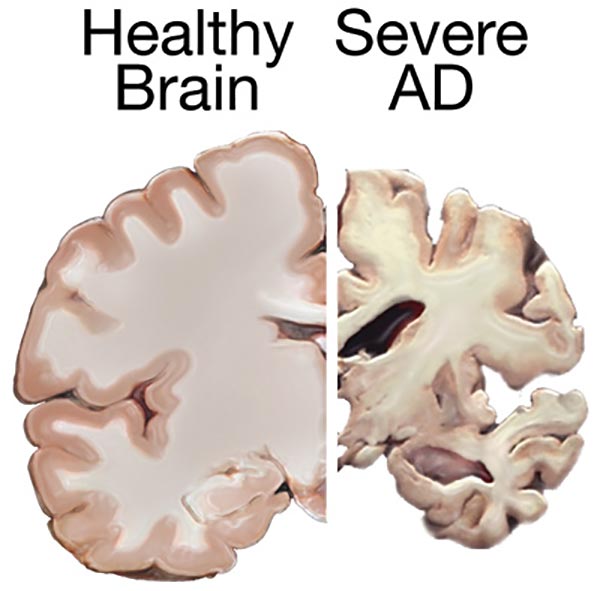
Healthy brain vs. brain with severe Alzheimer's Disease. Credit: National Institute on Aging/National Institutes of Health
Studies in Canada as well as the Netherlands, Sweden and elsewhere in Europe also suggest that dementia risk has declined in the past few decades. In the U.S. Langa and colleagues reported in Alzheimer’s & Dementia that the percent of adults over 70 years of age with cognitive impairment dropped from 12.2 to 8.7 between 1993 and 2002. The seniors were part of an ongoing longitudinal study funded by the National Institute on Aging (NIA), which surveys a representative sample of 20,000 older adults in the U.S. every two years.
But other research does not underscore this trend. A study led by Denis Evans, director of the Rush Institute for Healthy Aging in Chicago sends a more sobering message. The researchers measured new cases of Alzheimer’s between 1997 and 2008 and found no change in disease risk over time. Another study estimated, based on U.S. Census Bureau data, that the number of people with Alzheimer’s will nearly triple by 2050—and the percentage of seniors with dementia will creep upward.
All things considered, Langa agrees it’s very likely that due to higher life expectancy the absolute number of people with Alzheimer’s and other dementias will go up in the coming years. He notes, however, if an older adult’s risk for dementia continues declining as it has in some high-income countries over the last few decades, “that increase in number of cases may be a little less eye-popping than it would be if the risk were staying the same.”
The different results could have come from different starting assumptions—Evans assumes the number of new dementia cases will stay the same in coming decades, while Langa takes into account the possibility that dementia risk could decline because of changes in lifestyle and health prevention measures in the last quarter century.
What could be driving the apparent downward trend in dementia frequency? Although the question cannot be answered definitively, other analyses have linked lower dementia risk to better control of cardiovascular risk factors such as hypertension and high cholesterol, and by building up “cognitive reserve” with more education. People with chronic health conditions, however, add additional complexity to the picture. Those with type 2 diabetes, for example, are at higher risk for dementia. In light of rising levels of diabetes—as well as obesity—it’s possible these conditions could offset or override the downward dementia trend going forward, Langa says.
Epidemiological studies such as these could be further complicated by an artificial rise in reported dementia cases due to several factors. One is simply a growing awareness of Alzheimer’s disease. As a result, physicians may be more likely to make a diagnosis today, compared with decades ago, even in someone with the same level of cognitive impairment. They may also be more prone to list Alzheimer’s as a cause of mortality on death certificates. Second, neuroimaging and basic science research aimed at identifying potential treatments is shifting the field’s focus to earlier in the disease trajectory, driven by the belief that interventions stand the greatest chance in people who have not become too impaired. There is yet no cure for Alzheimer’s, although some drugs can alleviate symptoms. “From a clinical point of view, the concept of dementia syndrome has changed,” Brayne says. “Using current criteria, people get diagnosed at a much earlier stage.”
Despite the possible influence of growing disease awareness and changing diagnostic standards, bigger problems with assessing dementia rates could be methodological, says John Haaga, NIA deputy director for behavioral and social research. Different labs use different measures; the same group might use two measures 15 years apart. “How much change is real and how much is due to measurement differences?” Haaga says.
Evans sees a more fundamental problem with epidemiological studies of chronic disorders in older people. Although the diseases are scored in a binary fashion—you have it or you don’t—their underlying causes are often a continuous process. “When you diagnose Alzheimer’s disease, what you’re doing is placing a cut point on a bell-shaped curve” of cognitive function, Evans says. “You’re cutting off one tail to separate ‘Alzheimer’s’ from ‘non-Alzheimer’s.’” Putting the cut point in the same place every time is challenging. Well-trained researchers “will vary in how they do it,” Evans says. Yet because it is a point in the curve where the slope is changing sharply, even “a slight difference in where they place the cut can make a big difference in the number of people in the tail.”
On the whole, though, Haaga thinks the epidemiological data on dementia is improving. Whereas in the past “we were often extrapolating from small samples,” he says, “we’re now starting to be able to talk confidently about what the trends are in national populations.” Plus, efforts are underway to harmonize data sets, which should make it easier to compare results across different studies. That will become especially important as data comes in from other parts of the world—such as developing countries where the relative growth in dementia cases is predicted to exceed that of high-income nations.
Two thirds (66 percent) of people with dementia live in low- and middle-income countries, where less than 10 percent of population-based research has been conducted. Aptly named, the 10/66 study is investigating dementia and aging trends in these very regions. In India, for example, people do not live as long as they do in many developed countries, but life expectancy is continuing to go up, prompting a sharper rise in the number of dementia cases among the elderly. “In order to get Alzheimer’s or other dementias, you have to live long enough,” Langa says.
But changes in average life span can have different effects on different diseases. Eileen Crimmins, a gerontologist at the University of Southern California, studies how life expectancy influences chronic disease burden, as measured by the time one needs help and care. Two factors contribute to this: changes in mortality and changes in disease onset. “It is possible to end up with more people sick for a longer time when you are delaying death,” Crimmins told Scientific American via e-mail. “This is what has happened with heart disease.” More people in the U.S. are living with heart disease today, compared with decades ago, even though rates of death due to heart disease have gone down. Mortality and disease onset trends have played out more favorably for dementia, however. Nowadays fewer people have cognitive impairment, and people are not living as long with cognitive impairment, Crimmins says.
Crimmins, Brayne and Langa will discuss the research on falling dementia risk in a February 13 panel at the annual meeting of the American Association for the Advancement of Science in Washington, D.C. The trend is “intriguing and wonderful,” says NIA’s Haaga, who will moderate the panel. However, “I don’t want to give the impression that somehow the problem is now solved.” Even if progressively smaller percentages of the growing elderly population develop dementia in years to come, Haaga says, Alzheimer’s “is already the most expensive disease in the U.S., and it will continue to grow.”
Worldwide, the cost of dementia in 2015 was estimated at $818 billion. By 2030, it is expected to become a $2-trillion disease. As far as individual risk is concerned, however, “things are not getting worse,” Crimmins says. “Even if it is only a start of a trend, the likelihood of your getting dementia is getting smaller.”
