Scientists have been trying to grow human organs—including kidneys, livers, skin and guts—from scratch well over a decade.These “organoids” are not fully formed functional organs but miniaturized versions that help researchers model various diseases and test therapies.
It may sound like B-movie pulp, but now scientists have grown a mini brain with neural activity similar to that seen in a preterm infant. Previous efforts had grown stem cells into brainlike collections of neurons, but none demonstrated brain activity mimicking the real thing until now. An organoid functioning like an actual brain could help scientists study a range neurological and psychiatric disorders, such as epilepsy, stroke and schizophrenia.
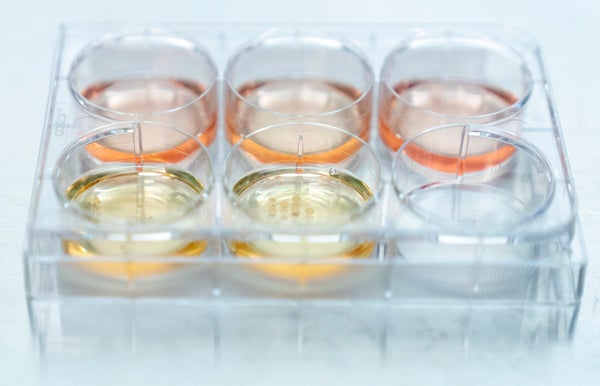
To grow its organoids, a team at the University of California, San Diego, used human induced pluripotent stem cells. These are cells taken from adult skin or blood that have been reprogrammed into stem cells, which can then be grown into just about any cell in the body, such as kidney or liver cells—or, as in the new study, neurons in the cortex, the part of the brain that controls complex thought and behavior. Scientists achieve this transformation by bathing the stem cells in a solution containing the right cocktail of transcription factors, molecules that guide fetal development by regulating how genes are turned on or off. The U.C. San Diego researchers have honed this process by developing a growth cocktail that allows their mini brains to develop for longer periods of time than in previous studies. Among the hundreds of cortical organoids they cultivated, many were still viable after nearly a year.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
As the organoids developed, the team used tiny electrodes to measure any electrical activity they generated. After just two months, the researchers detected scattered brain-wave activity of roughly a single frequency, much like that seen in the immature human brain. By 10 months out—when each organoid was about the size of a pea—the mini brains’ activity zapped at a range of different frequencies and became more regular, just as it does in the maturing human brain as new neuronal connections are made. This finding implies that through development, the organoids were establishing functioning synapses, the connections between neurons that allow them to communicate and generate movement, sensation and thought.
“The most exciting aspect was to see [so] much activity coming from something that is just a fraction of the human brain,” says Alysson Muotri, the new study’s senior author and a biologist at U.C. San Diego. Up to now, most scientists would have said that result would be impossible to achieve in the lab, he says.
Muotri explains that in many neurological and psychiatric conditions, the brain is physically intact, yet impaired neuronal circuitry results in disease. He believes cortical organoids could help scientists study such disorders of neural wiring, which include autism, epilepsy and schizophrenia.
“These are really interesting findings,” says Christof Koch, chief scientist and president of the Allen Institute for Brain Science in Seattle and a member of Scientific American’s board of advisers, who was not involved in the study. “The field is moving very rapidly, but this is much more than people have done so far. It’s pretty cool.”
Koch says the clinical potential of cortical organoids is vast. They can be used to model diseases and test various therapies while lessening the need for human and animal research subjects in early trials. And the San Francisco–based company System1 Biosciences is doing just that in hopes of developing new treatments for disorders of the brain. Additionally, Koch believes that organoids could be used to replace lost or damaged brain tissue. “In principle, if you lost a piece of brain due to things like a stroke, a gunshot or dementia, organoids could be used to replace that tissue and relearn brain function,” he says.
Organoid researcher Jürgen Knoblich, who was also not involved in the new work, agrees that the new findings are a major step toward more efficiently identifying promising treatments worth moving into animal and human studies. Yet “we also need to be careful when interpreting experiments like this,” he cautions. “The comparisons to real human fetal brains are viewed skeptically by some scientists.” Knoblich, interim scientific director of the Institute of Molecular Biotechnology in Austria, further notes that electrode recordings in the study only provided two-dimensional readings of brain activity, whereas three-dimensional data would be much more telling.
Cultivating humans’ most sophisticated organ—the seat of our thoughts, personalities and behaviors—in a small plastic dish might be morally troubling for many. But for now, Koch is not too concerned with the obvious ethical issues that come with growing something approaching a brain: “To be clear, no one would confuse these with an actual brain,” he says. “They [almost certainly] don’t feel anything,” because they lack neurons for sensing pain and the circuitry for processing it. He points out that such organoids have no vascular supply, so they could not grow much bigger than those in Muotri’s study.
Yet this restriction could change as stem cell engineers are able to generate larger and larger “brains.” What if they do start to feel something? Will they be distressed? Or, worse, in agony? And how would we know?
“Once you’re conscious, you’re not an object anymore; you’re a subject. Scientists need to do this in a way that avoids any suffering unless it’s in the service of something higher, like, say, a mouse model of curing cancer,” says Koch, who has advocated for reducing harm to animals on the basis that they are conscious and capable of feeling pain.
In the 1983 cult-classic film The Man with Two Brains, Steve Martin’s character—a neurosurgeon named Michael Hfuhruhurr—falls in love with a disembodied brain in a jar named Anne. Knoblich does not fret about such a Frankensteinian farce happening anytime soon, however. He believes cortical organoids will be used to model different aspects of brain function rather than to mimic an entire brain. “Any implication that those organoids are ever going to reach the complexity of a real human brain, in my view, is misleading and a dangerous overstatement of what I feel is otherwise a very exciting field,” he says.
But undoubtedly, as organoid technology advances, academic ethics committees will be busy for quite some time.