A promising technique to prevent mothers from passing on devastating mitochondrial diseases was thrown a biological curve ball this week: A paper published Wednesday in Nature shows that such diseases can come back to sicken a child, even when 99 percent of the mother’s own mitochondria are eliminated.
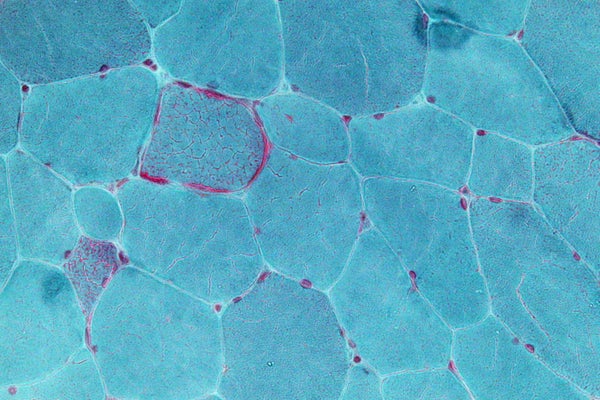
Mitochondria are the tiny power plants that provide the energy every cell needs to function. When a large percentage of these organelles malfunction, cells cannot do their jobs—and everything from weakness to death can result. Mothers with certain conditions may have such low levels of faulty mitochondria that they have no symptoms, but their kids can inherit a higher burden of these defective mitochondria, leading to devastating illness.
In attempt to combat this problem, researchers have essentially been—as one doctor described it—taking the “yellow part” of a mother’s egg and inserting it into the “white” of a donor’s egg. Because the child ends up with DNA from its mother, father and a donor, this mitochondrial replacement therapy has been nicknamed the “three-parent baby” technique. An apparently healthy boy was born using the approach in April in Mexico. He carries about 1 percent of his mother’s mitochondria, which if allowed to pass to him in full might have caused Leigh syndrome, a severe neurological disorder that is generally fatal in early childhood. His parents had two previous children who died of the disease, one at age 6 and one at 8 months, New Scientist reported.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
But the new laboratory study shows that the mother’s mitochondria can sometimes replicate faster than the donor’s and come to dominate again, potentially bringing disease with it. Still, that effect is likely to be rare, says Shoukhrat Mitalipov, the developmental biologist who led the research and has used the technique on mice and monkeys, reportedly without seeing any health problems. Mitalipov and Paula Amato, a reproductive endocrinologist also at Oregon Health & Science University in Portland, said at a news conference that they think mitochondrial replacement therapy should be tested in a clinical trial—despite concerns about the mother’s defective mitochondrial DNA making a comeback. “Because these diseases are so debilitating and often fatal and there are no cures, we think it’s still worth trying to move this research forward to prevent those diseases if we can,” Amato says. Congress currently bans such three-parent procedures for clinical use in the United States, but the United Kingdom has approved a similar technique that would allow even more of the mother’s mitochondria to be passed on to the child and a trial could likely be conducted there, Mitalipov says.
Although mitochondrial diseases are fairly rare, affecting about one in 5,000 children, Mitalipov and Amato say the three-parent technique could theoretically also be used to treat infertility and help with some stem cell treatments. Mitochondria (which have their own DNA, separate from the DNA in a cell’s nucleus) are inherited solely from the mother. Some consider the three-parent procedure controversial because of this mix of DNA, and because scientists worldwide have agreed to avoid making changes to human genetic inheritance.
A number of experts have also argued that mitochondrial replacement therapy is too little understood to try in people. Klaus Reinhardt, an evolutionary biologist and zoologist at Germany’s Technische Universität Dresden, thinks the mismatch between the donor’s mitochondrial DNA and mother’s nuclear DNA could cause mitochondrial problems in about one in 50 children born using the three-parent process. Inherited together, the nuclear and mitochondrial DNA can resolve each other’s defects. But when they come from different people, this mismatch can create problems for the child, says Reinhardt, who was not involved in the new research. The human genome, he explains, has 6 billion pairs of DNA and mitochondria have about 16,000, making it very challenging to predict their interactions. “We have no idea who ‘talks’ with whom,” he says.
Dan Mishmar, a mitochondrial evolutionist and geneticist at Ben-Gurion University in Israel, who was not involved in the new study, says his own research shows large differences between the mitochondrial genomes of Africans and Caucasians. When the parents’ DNA match their mitochondrial DNA, these gaps don’t matter, he says. But he worries about taking the mitochondrial DNA “out of context” when the donor and the mother have very different ethnic and racial backgrounds. Like Reinhardt, he worries that the DNA mixture itself could cause illness. “If you reduce the compatibility, you increase the susceptibility to complex disabilities, such as diabetes, Parkinson’s and … Alzheimer’s. That’s the thing we are afraid of.” But Mitalipov believes such problems can largely be avoided by matching the mitochondrial DNA of the mother with that of the donor, in much the same way that organ donors are matched to recipients by immune type.
Juan Carlos Izpisua Belmonte, a stem cell scientist at the Salk Institute in California who worked on the paper with Mitalipov, suggests an additional way to reduce the risks. He says his lab has developed a technique to cull mutant mitochondria from a mother’s egg before its nucleus is transferred to the donor’s. Reducing levels of the dangerous mitochondria should limit the number that reach the child, he adds.
For the new study, four women whose children had mitochondrial diseases underwent hormone therapy typically used for in vitro fertilization and provided eggs. Researchers took the DNA from the nucleus of these egg cells and transferred it into donor egg cells whose nuclei had been removed, a process called spindle transfer. The eggs with the mother’s nuclear DNA and the donor’s mitochondrial DNA were fertilized and allowed to divide and grow for five days. Then the embryos were turned into embryonic stem cells, ending their potential for development. These stem cells were transformed into brain, heart and other types of cells to see how their mitochondria would behave. In cells from one mother, the mitochondria reverted to the mutant type that she carried before the spindle transfer.
Although the new study raises questions about the safety of mitochondrial replacement therapy, Belmonte says it should also quell any fears that the research is moving too quickly. “We have to be convinced in the laboratory that we have done every possible experiment to make sure this is safe—as safe as we can [make it],” he says. “This is a wonderful way to avoid diseases, but we found a problem and we need to make sure we have ways to minimize or solve that problem before we go into the clinic.”