If there were a battle hymn against antibiotic resistance, it would have one common refrain: Every inappropriate prescription or insufficient dose strengthens the enemy. It may kill weak bacteria but it won’t eliminate stronger, drug-resistant ones that can move in and multiply. Eventually those robust microbes can outsmart available drugs, and even pass on survival instructions to other bacterial strains.That’s why most doctors—along with the World Health Organization and the U.S. Centers for Disease Control and Prevention—urge patients to always complete prescribed drug courses, even after they feel better. Taking too small a dose or stopping early, they reason, could fuel surges in drug resistance.
But a group of U.K. infectious disease experts is urging physicians and public health experts to change their tune. In a commentary published Wednesday in the British Medical Journal, they wrote, “The ‘complete the course’ message has persisted despite not being supported by evidence and previous arguments that it should be replaced. ... Nevertheless, there is evidence that, in many situations, stopping antibiotics sooner is a safe and effective way to reduce antibiotic overuse.”
The authors—Martin Llewelyn, a professor of infectious diseases at Brighton and Sussex Medical School, and nine British colleagues—point to recent studies that have shown shorter courses of certain drug classes such as quinolones are as effective as the longer courses that have been recommended in the past.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Yet the authors are not just calling for more studies that might lead to shorter standard treatment courses. They are saying that in the short-term the “always complete the course” message should be dumped. “Research is needed to determine the most appropriate simple alternative messages, such as stop when you feel better,” they wrote. They assert that there is also no evidence strong enough to support many of the current guidelines, a situation that forces physicians to rely on assumptions or historical practice to decide antibiotic treatment.
Drug resistance experts applauded the suggestions to reduce unnecessary medication use and to improve standard treatment protocols when possible. But they were skeptical about changing the “finish your pills” messaging or significantly altering outpatient care. “My thought is that this is a radical stance—although in some ways correct,” says Lance Price, a microbiologist and director of the Antibiotic Resistance Action Center at The George Washington University. “This [commentary] is a really good thought piece, but I think they go too far in saying we need to stop this messaging. We know antibiotics are not smart bombs or snipers—they do not target only one desired body part like the bladder, as we would like. But to say, ‘Let’s pull the plug on this messaging without providing a reasonable, actionable countermessage’ is totally irresponsible.”
Lauri Hicks, director of the Office of Antibiotic Stewardship at the CDC, says she agrees that there are many unanswered questions about appropriate drug treatment courses. But she cautions that patients should not stop taking their prescribed antibiotics on their own. “I recommend that if a patient is feeling better while taking a course of antibiotics, that the patient or the patient’s family should consult a physician to see if those antibiotics can be safely stopped,” she says. “I think it really needs to be a decision made with input from the provider. In certain circumstances taking the full course is important, and it may not be as important for some other, milder infections.”
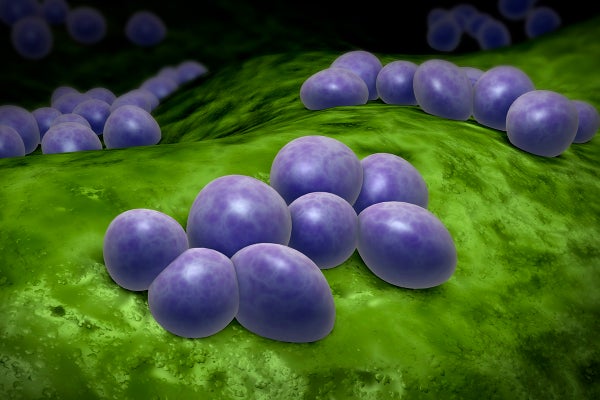
Bacteria have developed multiple tactics to boost their resistance, depending on the infection and antibiotic involved. Some strains have learned how to expel an antibiotic before it can do any damage. Others can effectively neutralize an antibiotic by changing it in a way that makes it harmless to them. In some cases bacteria have mutated to change their outer structures so an antibiotic cannot recognize them or attach to them—rendering the drug useless.
Longer courses of antibiotics put selective pressure on bacteria in the body, which can help the microbes’ resistance grow. As a result, infectious disease experts currently try to find a balance between making sure drugs are effective at knocking out harmful bacteria while keeping the treatment duration to the bare minimum required to stamp out an infection. The Infectious Diseases Society of America (IDSA) has changed some of its guidelines for certain medications, based on recent studies that show shorter courses suffice. But some studies indicate shortening treatment courses would leave patients vulnerable to a resurgence of infection or, in some cases, potentially result in selective growth of resistance organisms.
Existing recommendations are largely based on clinical trials, says Helen Boucher, a professor of medicine and infectious diseases at Tufts Medical Center and a spokesperson for the IDSA. “I think the spirit of this paper is very much in line with what IDSA advocates for,” Boucher says. “As part of the strategy to combat the antibiotic resistance crisis, we should think about strategies to use less drugs and use drugs for shorter duration.” The incentive to study these shorter courses needs to come from funders like the National Institutes of Health, she adds.
Llewelyn and his co-authors suggest some specific steps for the path forward. They wrote that a common practice in hospitals—a daily review of a patient’s continued need for antibiotics—must become more common in primary care as well, because that is where some 85 percent of prescriptions are written. (Many experts, including Hicks, say this recommendation is probably unrealistic due to the need to pay for follow-up visits and limitations on both doctors’ and patients’ time in an outpatient setting.) The authors also call for fundamental changes in public health and drug treatment messaging: “Public education about antibiotics should highlight the fact that antibiotic resistance is primarily the result of antibiotic overuse and is not prevented by completing a course,” they wrote. Such big changes in messaging are not yet ready for prime time, Price says.
No current guidelines suggest stopping drug treatment partway through a recommended treatment course. For example, the CDC has often said in its public materials and reports, “Take antibiotics exactly as the doctor prescribes. Do not skip doses. Complete the prescribed course of treatment, even when you start feeling better.” But the CDC and IDSA say they are continually reviewing the literature and support guidelines based on new information.
Changing standard prescribing practices will likely be challenging, the commentary’s authors acknowledge, pointing to the “finish your drugs” education in U.K. schools. “The idea is deeply embedded, and both doctors and patients currently regard failure to complete a course of antibiotics as irresponsible behavior,” they wrote. Even designing experiments to test reducing antibiotic courses remains difficult, they added, because participants are often invited to consent to receive shortened antibiotic treatment on the basis that this could reduce the risk of antibiotic resistance—yet they are “taught from school that it increases this risk.”