Editor's note: Catherine Spong's title was changed to reflect her position as acting director of an NIH institute on May 16.
For most people, a Zika virus infection brings little more than a slight fever or a mild rash. But when the mosquito-borne illness strikes during pregnancy, it can set off a slew of devastating birth defects that include microcephaly (a dangerously small head and brain) as well as hearing and vision loss. The one barrier that lies between Zika lurking in a mother’s bloodstream and the health of her unborn child is the placenta, a short-lived organ that has been hard to study. Now a cadre of specialists have developed new methods to examine the organ, spurred on by the need to learn how Zika crosses this normally impenetrable barrier.
The placenta is remarkable. It rapidly materializes during pregnancy—supplying the baby with nutrients and oxygen, clearing waste, churning out hormones and fending off infections—before making a bloody exit via the afterbirth. Much of what we know about the human placenta comes from research on this discarded pound of flesh, which requires a kind of finesse found in few labs across the country. The trouble is, these decaying, disk-shaped masses provide just a glimpse of their former selves, much like a cadaver conveys mere bits and pieces of a person’s earlier life.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Many scientists felt no urgency to find out more. “I always like to think of the placenta as the engine of your car,” says Carolyn Coyne, a virologist at the University of Pittsburgh. “When you drive to work in the morning, your engine doesn’t usually cross your mind. But if it breaks down, then you care. Same thing when you're pregnant, you're thinking, of course, about your baby, not the placenta and all the work it’s doing. Unless something goes wrong.”
Coyne started thinking seriously about the placenta when she became pregnant with her son, seven years ago. She wondered if she could harm her baby by continuing to handle viruses in her lab. So she ran a quick Google search and was troubled to find how little was known about the vital organ.
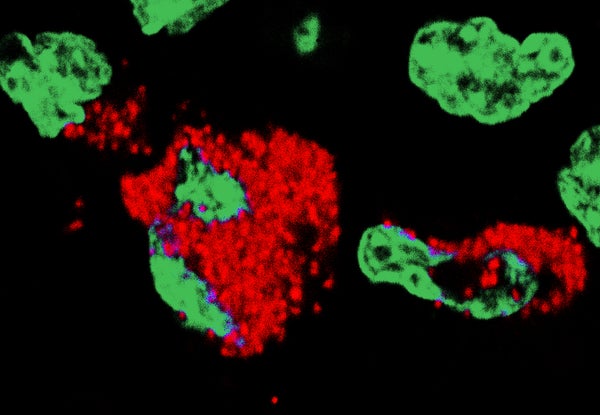
The human placenta can keep most, but not all, maternal infections from causing birth defects. But how does it accomplish that feat and shield the developing fetus? Soon after the Zika outbreak began Coyne harvested cells from full-term placentas and exposed them to different strains of the virus. She discovered the cylindrically shaped cells called trophoblasts that envelop the placenta exude potent molecules called interferons that usually protect them from infection. When she added the trophoblasts’ interferons to other types of cells that inhabit the placenta, like fibroblasts or endothelial cells, those cells suddenly became resistant, too.
Yet multiple studies have detected traces of the Zika virus in the brains and amniotic fluid of affected babies. Unfortunately, cells from old placentas deteriorate too rapidly for Coyne to use them to investigate the way Zika manages its break-in. One possible solution is to use repeatedly dividing placental cells, which in theory could be studied for eternity. To better mimic the dynamic three-dimensions of real life, Coyne took these cultured, immortalized placental cells for a little spin. She tacked cultured trophoblasts and their companion blood vessel cells onto tiny beads. Then she spun the beads around using an instrument from NASA called a rotating wall vessel bioreactor. It generates a zero-gravity environment.
Coyne says the cells end up floating and whirling around in their growth media, subject to the same shear stress and rotational forces found in a mother’s womb, like sea anemones exposed to the onslaught of ocean currents. In contrast to cells grown flat on their backs in lab dishes, the cells cultured in three dimensions resist infection by the parasite that causes toxoplasmosis, behaving like cells from a live placenta. Now she is using the new 3-D model to recreate a Zika infection, testing the hypothesis that reducedlevels of interferons might allow Zika to infiltrate placental cells. Coyne thinks that some placentas, in some women, might produce less interferons, putting their babies at higher risk.
A recent study in animal models underscores the role of these protective factors in Zika infection. Indira Mysorekar, a microbiologist at Washington University School of Medicine in Saint Louis, reported last week in Cell that mice engineered to be genetically or chemically deficient in interferons were more vulnerable to the damaging effects of Zika. She found that unlike other viruses like dengue, Zika appears to possess a unique predilection for the placenta. It pushes through multiple cellular barriers to reach the fetus, damaging the placenta along the way and prompting fetal demise in the most severe cases.
Mysorekar explains that the Zika virus seems to follow a kind of molecular homing signal on its path from mother to child. “It may be just one or two viruses that get through, but once they're in they are able to replicate. The cells are full of viruses,” she says. “It’s scary.”
Although the mouse models in Mysorekar’s study mirrored many aspects of human Zika infection, they lacked two of Zika’s most devastating impacts: brain calcifications and microcephaly. Because nearly every placental mammal has its own unique placenta, the only way to know for certain what is happening in a person is to study one. Catherine Spong, a maternal fetal medicine specialist and acting director of the Eunice Kennedy Shriver National Institute of Child Health and Development, says work is already underway to adapt old technologies and invent new ones that can follow the human placenta as it grows, develops and functions alongside the fetus. But these approaches are years away from realization, providing little reassurance to women faced with the current Zika outbreak. As mosquito season quickly approaches, the virus will likely infect more women and endanger more babies.
Vikki Abrahams, a reproductive immunologist at Yale University, says scientists are only beginning to appreciate the ramifications of emerging infectious diseases like Zika. Even when these pathogens are unable to infect the placenta, they can still trigger a dangerous inflammatory response from the immune system that may lead to problems lasting well beyond pregnancy, including autism, schizophrenia, lower IQ and impaired social skills.
“It is not just nine months,” she says. “If we don’t have a good understanding about basic pregnancy and the basic questions about how the placenta functions, then we can’t understand when things go wrong or how to stop problems that arise, and the damage to mother and offspring will continue to perpetuate. It becomes a global problem affecting the general population.”