About 100 times rarer than Parkinson’s, and often mistaken for it, progressive supranuclear palsy afflicts fewer than 20,000 people in the U.S.—and two thirds do not even know they have it. Yet this little-known brain disorder that killed comic actor Dudley Moore in 2002 is quietly becoming a gateway for research that could lead to powerful therapies for a range of intractable neurodegenerative conditions including Alzheimer’s and chronic traumatic encephalopathy, a disorder linked to concussions and head trauma. All these diseases share a common feature: abnormal buildup of a protein called tau in the brains of patients.
Progressive supranuclear palsy has no cure and is hard to diagnose. Although doctors may have heard of the disease, many know little about it. It was not described in medical literature until 1964 but some experts believe one of the earliest accounts of the debilitating illness appeared in an 1857 short story by Charles Dickens and his friend Wilke Collins:
“A cadaverous man of measured speech. A man who seemed as unable to wink, as if his eyelids had been nailed to his forehead. A man whose eyes—two spots of fire—had no more motion than if they had been connected with the back of his skull by screws driven through them, and riveted and bolted outside among his gray hair.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
He had come in and shut the door, and he now sat down. He did not bend himself to sit as other people do, but seemed to sink bolt upright, as if in water, until the chair stopped him.”
Nearly a century later Toronto neurologist Clifford Richardson noticed similar characteristics in several of his patients and in a business executive who was his good friend. Richardson asked his colleague Jerzy Olszewski and John Steele, a trainee, to help him examine additional cases. The trio reported their findings at a neurology research convention in 1964, where the disease was christened “Steele–Richardson–Olszewski syndrome.” The illness was later renamed progressive supranuclear palsy (PSP) to describe the weakness or paralysis (palsy) patients develop when brain areas that control eye movements are affected by the syndrome—which produces the classic symptom of motionless eyes described by Dickens. In addition, people with PSP lose the sense of balance, although unlike in Parkinson’s they fall backward instead of forward. Many PSP patients also struggle with speaking and swallowing.
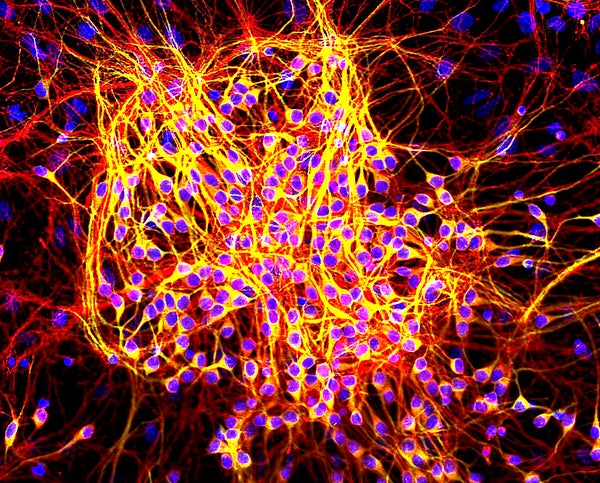
The problems can be traced to loss of nerve cells in the brain areas responsible for those capabilities—such as the basal ganglia, brain stem and cerebral cortex. Under a microscope these are the very regions that accumulate tangled clumps of tau, a normal protein found mostly in neurons. It binds to structures called microtubules, which help move nutrients up and down the cell. But in PSP and related disorders something goes wrong: Tau proteins twist out of shape and start sticking to one another rather than stabilizing microtubules. Then, through a mysterious process, the tau clusters leave the cell, spread throughout the brain and muck up communication between neurons. “If we could prevent tau from accumulating, it could be a potential treatment,” says David Holtzman, a neurologist at Washington University in Saint Louis (W.U.).
Beyond PSP, other brain diseases are also marked by abnormal tau clumps—among them a rare movement disorder called corticobasal degeneration, an inherited form of frontotemporal dementia with Parkinson’s-like features, and Alzheimer’s disease.
Research on Alzheimer’s has focused largely on another protein called amyloid beta, which clusters into “plaques” in the brain. But there is growing interest in tau’s role. Whereas analyses of the brain were once limited to autopsy samples at the time of a person’s death, advances in an imaging technique known as positron emission tomography (PET) now enable researchers to detect amyloid and tau in the brains of living people. And recent PET studies offer intriguing insights into how these signature proteins relate to each other and to cognitive decline in the earliest stages of Alzheimer’s.
PET scans have not been widely adopted as a clinical tool but are used in research, which clearly shows amyloid starting to clog the brain some 10 to 15 years before a person shows noticeable memory loss. Roughly a third of older people live with heads full of amyloid—about as much as someone with Alzheimer’s—even while showing no cognitive problems. Some will eventually develop dementia. Yet “we cannot predict when, or even if, they will,” says William Jagust, a neuroscientist at the University of California, Berkeley.
Nevertheless, many in the field remain hopeful they can keep disease at bay in these “on the verge” patients with therapies that reduce the presence of brain amyloid. Such approaches have not proved clinically effective, although it could be that the amyloid-lowering drugs were tested on the wrong people—participants with Alzheimer’s too advanced to be remedied or cognitively impaired seniors who turned out not to have brain amyloid. Several large trials of amyloid-based therapies are underway in groups of people more carefully selected to be at high risk for Alzheimer’s. But even if those therapies pass muster, they would need to be given very early before people develop memory problems, says neurologist Adam Boxer of the University of California, San Francisco. “That’s really tough, because many of our patients already have symptoms, so what do we do for them?”
A PET study Jagust’s team recently published in Neuron indicates that tau—more than amyloid—could be key for determining when to intervene, and in whom. The researchers analyzed healthy young adults, healthy older adults and older adults diagnosed with “probable Alzheimer’s.” Those with a lot of tau in the temporal lobes and neocortex—brain areas important for sensory perception and memory—were close to dementia onset whereas symptoms could still be years out for people with high amyloid. Tau collects in other brain areas as part of the normal aging process but appears to spell trouble when found outside of memory centers, Jagust says.
An analysis reported last month in Science Translational Medicine bears out this idea. Researchers at W.U. conducted amyloid and tau PET scans on 36 healthy seniors and 10 with mild Alzheimer’s. Examining the brain scans in the context of other disease markers from spinal fluid analyses and neuropsychiatric tests on the same participants showed that the rise and spread of tau in the brain tracked more closely with declining mental function than did amyloid. Location seems critical, too. Whereas amyloid may show up in various brain areas, tau appears more restricted to regions associated with the cognitive deficits.
These data support the emerging view that “amyloid beta is the trigger but tau is the executioner,” says Karen Duff, a cell biologist who studies neurodegenerative diseases at Columbia University. Amyloid may be a driving force that sets off the tau misfolding and clustering, but beyond a certain point the toxic tau clumps self-propagate “and you can’t rein them in,” Duff says. And because tau more closely aligns with the start of dementia, an effective therapeutic has “probably got to deal with the tau,” she adds.
Years ago W.U.’s Holtzman and former colleague Marc Diamond, who has since moved to the University of Texas Southwestern Medical Center, identified tau-binding antibodies that slow the spread of toxic tau clusters in a lab assay using cultured cells. When injected into mice engineered with a tau mutation that makes the protein clump abnormally in brain cells, triggering memory and motor problems, the antibodies reduced the clumping and improved the animals’ behavior. The antibody has entered human testing.
Other approaches aim to decrease tau protein production by targeting RNA; blocking tau clustering by interfering with chemical modifications on the protein’s surface; or binding microtubules in order to enhance a normal tau function that gets lost as the protein misfolds and aggregates. At present a few tau-targeting approaches are being evaluated in Alzheimer’s clinical trials. But more are being tested in people with PSP. Scientists are eager to assess tau therapies in PSP for a number of reasons: First, it is a pure tauopathy. Whereas people with Alzheimer’s can have tau as well as several other proteins clustering in their brains, PSP patients only have abnormal tau. Second, tau has a stronger genetic link to PSP than it does to Alzheimer’s. Among the DNA variants known to cause Alzheimer’s or increase risk of the disease, none are found in the tau gene. A large-scale genetic analysis in PSP patients, however, identified a common tau sequence that increases by 5.5 times a person’s chances of developing the disease, making this variant a stronger risk factor for PSP than one copy of the apolipoprotein E-ε4 variant is for Alzheimer’s. (Apolipoprotein E-ε4 is the top risk gene for Alzheimer’s.)
Other reasons for testing tau drugs in PSP patients have more to do with clinical trial practicalities. If an intervention is effective, then the participants taking the study drug should deteriorate more slowly than those in the placebo group. In some diseases such as Alzheimer’s, however, decline is slow and inconsistent to begin with. PSP, by comparison, runs its course more rapidly and predictably. Whereas it may require an 18-month trial in 1,000 to 2,000 patients to determine if a drug is effective for Alzheimer’s, “you probably only need six to 12 months and 200 to 300 patients for the same sort of power to detect a drug’s disease-modifying effect in PSP,” says U.C. San Francisco’s Boxer. Bottom line: conducting clinical trials in PSP is faster and less expensive. Also, because PSP is a rare disease, clinical trials for this condition are eligible for incentives that could enable faster drug approval by the U.S. Food and Drug Administration and European Medicines Agency.
With PSP so uncommon, researchers anticipated having a hard time recruiting trial participants. Yet enrollment has gone “better than expected,” says Boxer, who helps design and conduct clinical trials in PSP, Alzheimer’s and other brain disorders. Because there are no good drugs out there, he says, PSP patients “are incredibly enthusiastic to participate in trials.”