Researchers in the U.S. have begun editing the genes of adults with devastating diseases, using a tool known as CRISPR. China has already launched multiple trials of CRISPR in humans. Last year Chinese researcher He Jiankui caused a global outcry when he used the same tool to gene edit twin baby girls when they were just embryos. There is far less concern about other CRISPR trials either in the U.S. or China, in part because genetic changes in the adults treated will not be passed on to future generations. “If it’s done well and carefully, I’m not so worried, to be honest,” says Robin Lovell-Badge, a British geneticist and stem cell scientist, regarding the use of CRISPR in these new trials.
Even so, there are lingering questions about whether it is still too early to move ahead with the technology. CRISPR can, at times, inadvertently edit genes that were not intended to be altered. The fear is that such “off-target edits” could cause other health problems, including cancers. Lovell-Badge, a group leader at the Francis Crick Institute in England, says things can always go wrong, but CRISPR has been adequately vetted in laboratory research, and it is a reasonable time to test the tool in adults.
The fact that CRISPR went from an idea in a lab to a trial in people during this decade speaks to the elegance and versatility of the technology,” says Sam Kulkarni, CEO of the company CRISPR Therapeutics, which is in one of two groups testing CRISPR-based gene editing approaches in people.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The first trial of CRISPR in humans took place in China in 2016, when Lu You, a physician at Sichuan University, put gene-edited cells into a lung cancer patient. Since then, other Chinese trials have moved forward, though not much is known about them.
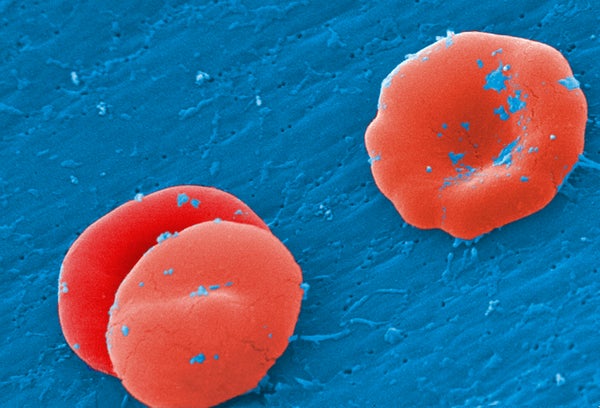
Early this year Kulkarni’s company, in collaboration with Vertex Pharmaceuticals, began testing CRISPR gene editing on patients with sickle cell disease and beta-thalassemia: researchers are editing genes in blood cells removed from each patient and then replacing them to restore normal hemoglobin, which transports oxygen throughout the body.
In late July pharmaceutical giant Allergan and genome editing company Editas Medicine announced that they were ready to enroll subjects in a clinical trial to treat one of the most common inherited form of childhood blindness, called Leber congenital amaurosis type 10. The companies claim that trial is the first to use CRISPR to edit genes inside the body. The eye is considered a relatively safe place to test the technology because changes made there should not affect other areas.
Several other gene-editing techniques besides CRISPR have already received federal approval, including Luxturna, for a different form of Leber congenital amaurosis, Zolgensma, for spinal muscular atrophy—a debilitating and often fatal degenerative muscle disease—and Kymriah, which has been approved for some blood cancers.
Both teams in the U.S. say they chose CRISPR because they believe it is the best tool for the job. Essentially a pair of molecular scissors, CRISPR (which stands for clustered regularly interspaced short palindromic repeats) comprises a family of DNA sequences and enzymes. Bacteria recruit CRISPR to snip the DNA of invading viruses. Using a molecular guide, the tool can break a strand of DNA, either knocking it out of commission or forcing a repair that corrects an inherited mutation.
“We have reasons that we are confident that the approach we’re taking has the potential to be something very valuable to patients,” says Vertex’s chief scientific officer David Altshuler. “We also continue to work on improvements to every aspect of what we’re doing.”
The gene edits made by Vertex and CRISPR Therapeutics will suppress a gene called BCL11A, which will restart production of fetal hemoglobin, a type of hemoglobin that helps fetal blood hold onto oxygen. Even people who inherit the sickle cell gene from both parents make fetal blood (or they would not have survived to birth), so reactivating fetal hemoglobin should allow them to lead normal, healthy lives, Altshuler says.
Those edits are made on blood cells that have been removed from the body and are then reinserted after the patient has undergone a procedure to clear out diseased blood precursor cells. The gene editing is transient, and the edited blood cells undergo quality checks before being reinserted, minimizing the risks of unintended gene edits, Altshuler says.
The edited cells then grow into the bone marrow and begin making healthy red blood cells that do not “sickle,” so they will not stick to the inside of blood vessels, cutting off circulation and causing dangerous pain crises. People born with sickle cell and a genetic fluke that allows them to keep making fetal hemoglobin do not suffer from the disease, research shows. And sickle cell does not recur in patients who get bone marrow transplants that allow them to make healthy blood cells—which is currently the only way to cure the disease but is available to only a small minority of people. Altshuler says this result gives him confidence that the gene edits can potentially provide meaningful and lifelong benefits to patients.
Editas’s chief scientific officer, Charles Albright, says his company also believes it will be able to provide a safe and effective treatment. “We did a whole bunch of preclinical studies that increased our confidence that we understood how to use the medicine and that we had a good chance of providing therapeutic benefit,” he says, citing a Nature Medicinestudy published by the company early this year.
Because the treatment is narrowly targeted to cells that perceive light, known as photoreceptors, any unintended gene edits should not cause widespread problems, Albright says. Patients will receive an injection behind their retina that will deliver the gene-editing machinery to the photoreceptors. The edit is intended to restore the gene’s proper function, and that correction will be passed on as the photoreceptors divide and create “daughter” cells.
“One of the great things about gene therapy and gene editing is you’re really going after the molecular defect in these patients,” Albright says. “If this works, it’s a cure. The reason to think that is we’re going after the underlying defect that caused the problem.”
The therapy is expected to be less effective in adults who have lived for years with limited vision; Editas plans to begin testing the approach in children as young as three after it has proved initial safety. The company will test three doses of the gene editing-machinery, treating one eye at a time for safety reasons, to see which dose provides the best results and fewest side effects, Albright says.
There are a number of reasons these trials are not causing the type of controversy that erupted last year with the twin baby girls. First, only edits to eggs, sperm and embryos can be passed down to future generations, so changes made for these clinical trials will stop with the patient. In the controversial Chinese study, He Jiankui edited the genes right after fertilization, changing every cell in the body, including the germ cells, so the girls’ own children can inherit whatever mutations they ended up with. (Scientists are still not sure whether there were unintended edits or how the changes—which were imperfect and inconsistent between the two—might affect the girls as they grow.)
Also, many researchers, including Lovell-Badge, have criticized He’s decision to edit the CCR5 gene, which can confer protection against HIV when people are born with both copies missing. The twins’ father has HIV, and He said he was trying to protect the girls from developing the virus. But there are other ways to prevent such transmission, Lovell-Badge says, and the edits made to the girls do not produce precisely the same genetic sequence as people born with the double mutation. In the current trials, both of the targeted genes are associated with serious diseases for which there are few good alternative therapies.
And finally, Lovell-Badge says, the work done by the two collaborations has been carefully vetted with years of animal research and guidance from the U.S. Food and Drug Administration. By contrast, He reportedly did not tell his hospital or research institution that he was conducting his experiments—which is considered a major breach of medical protocol. And the consent he received from the parents of the twins and another couple whose embryo he gene edited did not meet prevailing standards, researchers have said.
Early trials always carry some risk, Lovell-Badge notes. But major treatment advances depend on patients willing to take those risks. “It’s good that some patients are brave enough to try innovative steps to finding cures,” he says.