The global emergency triggered with the rapid spread of Zika has caused countries around the world to join forces in order to improve the knowledge of the virus and its processes. Two studies recently published in Cell showed, in experiments conducted on female mice, how Zika is able to cross the placenta, infect the fetus and cause microcephaly—insufficient development of the skull—in their offspring.
The first one, in Cell, led by researchers at Washington University School of Medicine in Saint Louis, establishes the first models on how Zika spreads from a pregnant mouse to her fetus. The results show how the virus invades and damages first the placenta, then the fetus. “There were doubts about the intrauterine transmission of Zika. Our data confirms that the virus crosses the placenta and may cause congenital problems, including the death of the fetus," says Michael Diamond, one of the scientists participating in this study.
Although mice are not normally susceptible to the virus, the team of researchers developed two models based on the immunodeficiency of the mouse in order to provide Zika with a more accessible entry route. In the first model the female rodents were genetically modified to have a defective immune system. In the second the animals received injections of an antibody that prevented the complete performance of their immune systems.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
In the genetically immunodeficient mice scientists observed that the viral load was 1,000 times greater in the placenta than in the mothers’ serum, which denotes, according to them, that Zika primarily infects this organ.
Once in the placenta, the virus begins to infect the cells of the trophoblast—the tissue that supplies nourishment to the embryo—and damages the blood capillaries of the fetus. “Previous work already showed that late-stage placental cells were resistant to infection; now our study shows that the virus is able to cross the barrier between the maternal tissue and the fetus," the scientists wrote in their paper.

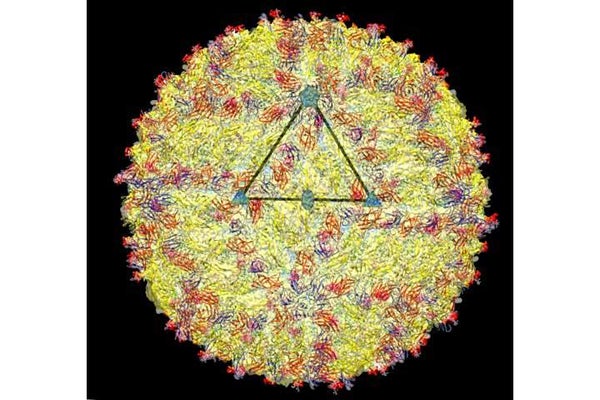
Differences in brain sizes of healthy versus infected mice.
Credit: Cell
Most of the fetuses died before birth, and those that managed to survive were born smaller and had Zika replications in their brains and central nervous systems. “The two models provide different aspects of biology,” Diamond says. “In the genetic model we see how this virus slows growth down, harms the brain and causes fetal death. The model with antibodies, which is less severe, helps us follow the development of the disease after birth,” he says.
These results fit with the second study in Cell Stem Cell, led by the Chinese Academy of Sciences’ Institute of Genetics and Developmental Biology and the Beijing Institute of Microbiology and Epidemiology, showing that the offspring of mice infected with the virus suffer from microcephaly at birth.
In this case, the virus was injected directly into the brains of the fetuses at the precise moment when neuronal progenitor cells proliferate rapidly and neurons begin to emerge.
The scientists were able to observe a reduction in the brains of the offspring afflicted with viral load. “The most surprising thing about this study is that although both neuron and neuronal progenitor cells were infected, almost all cell death focuses on the neurons indicating that these are more prone to virus-induced cell death,” co-author Zhiheng Xu says.
“Most of the time, the placenta is an effective barrier between mother and fetus but Zika has found a way to overcome this and spread through different layers of the trophoblast. We see the virus in the lining of the blood vessels of the fetus, then we see it in circulation, and shortly thereafter it is able to get to the brain,” says Indira Mysorekar of Washington University, a co-author of the Cell paper.
Researchers from both studies continue to analyze the models and work in identifying potential drugs that can reverse the microcephaly process caused by Zika. But they insist one should remember that mice are not people. Cheng-Feng Qin, a co-author of the Cell Stem Cell study at the Beijing Institute of Microbiology and Epidemiology, concludes that “we must be careful when it comes to extrapolating these results to the human model.”